SHANGHAI, China and PALO ALTO, Calif., June 9, 2015 /GlobeNewswire/ — Cellular Biomedicine Group Inc. (NASDAQ: CBMG) (“CBMG” or the “Company”), a biomedicine firm engaged in the development of new treatments for degenerative and cancerous diseases, today announced that it has entered into a definitive agreement to acquire from Blackbird Bio Finance (“BB”) University of South Florida’s (“Licensor”) next generation GVAX vaccine’s (“CD40LGVAX”) related technologies and know-how for an initial consideration of $2.5 million in cash and $1.75 million in shares of the Company’s Common Stock. The per share price will be based on the 20-day volume weighted average price (“VWAP”) of the Company’s Common Stock upon the closing of the acquisition. CBMG will pay potentially more than $25 million in future milestones and royalty payments. As part of the transaction, CBMG will be the exclusive global licensee of the Licensor’s related technologies and know-how, the progeny manufacturing rights with access to a master vaccine bank originating from the University of South Florida (“USF”).
The inventor of CD40LGVAX, Scott Antonia, MD, Ph.D. is currently the Department Chair of Thoracic Oncology and Program Leader of the Immuno-oncology Program at the Moffitt Cancer Center. Dr. Antonia ranks among the foremost experts in the world of immuno-oncology and is an active collaborator with large pharmaceutical companies. He is recognized as one of the world’s leading authorities in the treatment of lung cancer with immunotherapeutics and has recently joined the Company’s Scientific Advisory Board. Given the positive Phase I results of CD40LGVAX alone in non-small cell lung cancer (NSCLC), Dr. Antonia plans to combine the CD40LGVAX with a checkpoint inhibitor, anti-PD1 monoclonal antibody, Nivolumab, in a three patient lead-in Phase I clinical trial followed by a randomized Phase II clinical trial in the U.S. to evaluate the safety and efficacy of the combination in patients with Stage 4 unresectable non-small cell lung cancer. The clinical trials are expected to commence in the second half of 2015.
Via Krishan Maggon



 Your new post is loading...
Your new post is loading...








ABOUT CD40LGVAX
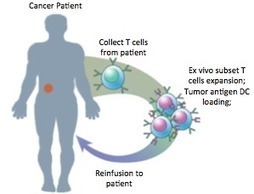
CD40LGVAX is a vaccine in which irradiated allogeneic lung adenocarcinoma cells are combined with a bystander cell line transfected with hCD40L and hGM-CSF. The key differentiator is the transfection of the bystander cell line with GM-CSF and CD40L. Both GM-CSF and CD40L can activate dendritic cells (DC). Nivolumab, an anti-PD-1 monoclonal antibody, enhances cytotoxic T cell activity by blocking the interaction between PD-1 and its receptors. The vaccine has previously been tested in a Phase I trial, and has shown encouraging efficacy and toxicity profile. In the United States, the Food and Drug Administration (“FDA”) has approved Nivolumab for treatment of patients with melanoma and advanced squamous NSCLC who have progressed on or after platinum-based chemotherapy. About 25% to 30% of all NSCLC are squamous. By combining CD40LGVAX with an anti-PD1 monoclonal antibody, the approach is expected to further boost the body’s immune system to kill cancer cells. Given the strength of both products and potential synergistic mechanism of action, this potential combination may provide more clinical benefit to NSCLC than either product alone.