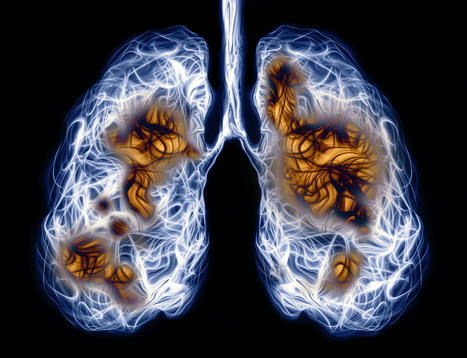
Repair of lung injury due to viral infection can be facilitated by nanoparticle-delivered mRNA targeting TGF-βR2 signaling. Respiratory infections, such as those caused by SARS-CoV-2 or influenza, can damage the lungs’ delicate network of capillary blood vessels, compromising oxygen delivery and carbon dioxide removal. To overcome this damage, the lungs depend on the regenerative capacities of vascular endothelial cells. As valuable as these cells are, they can, according to University of Pennsylvania scientists, benefit from a little help. The scientists, led by Andrew Vaughan, PhD, focused on a repair pathway involving vascular endothelial growth factor α (Vegfa) and the TGF-β receptor 2 (TGF-βR2). Using animal models and human tissue samples, the scientists showed that delivering Vegfa via lipid nanoparticles (LNPs) greatly enhances modes of repair for damaged blood vessels. “Mice deficient in endothelial Tgfbr2 exhibited prolonged injury and diminished vascular repair,” the article’s authors wrote. “Loss of endothelial Tgfbr2 prevented autocrine Vegfa expression, reduced endothelial proliferation, and impaired renewal of aerocytes thought to be critical for alveolar gas exchange.” “We developed a lipid nanoparticle that targets the pulmonary endothelium, Lung-LNP (LuLNP),” the authors continued. “Delivery of Vegfa mRNA, a critical TGF-βR2 downstream effector, by LuLNPs improved the impaired regeneration phenotype of endothelial cell Tgfbr2 deficiency during influenza injury.”
Vaughan’s team and other investigators had previously shown that endothelial cells are among the unsung heroes in repairing the lungs after viral infections. But Vaughan’s team noted that its work demonstrated that a “more granular understanding of the fundamental mechanisms driving reconstitution of lung endothelium” could inform efforts to facilitate therapeutic vascular repair. “Here we’ve identified and isolated pathways involved in repairing this tissue, delivered mRNA to endothelial cells, and consequently observed enhanced recovery of the damaged tissue,” Vaughan said. “These findings hint at a more efficient way to promote lung recovery after diseases like COVID-19.” The team found Vegfa’s involvement in this recovery, while building on work in which they used single-cell RNA sequencing to identify TGF-βR2 as a major signaling pathway. The researchers saw that when TGF-βR2 was missing, it stopped the activation of Vegfa. This lack of signal made the blood vessel cells less able to multiply and renew themselves, which is vital for the exchange of oxygen and carbon dioxide in the tiny air sacs of the lungs. “We’d known there was a link between these two pathways, but this motivated us to see if delivering Vegfa mRNA into endothelial cells could improve lung recovery after disease-related injury,” said first author Gan Zhao, PhD, a postdoctoral researcher in the Vaughan laboratory. The Vaughan laboratory then reached out to Michael J. Mitchell, PhD, of the School of Engineering and Applied Science, whose laboratory specializes in LNPs, to see if delivery of this mRNA cargo would be feasible.
“LNPs have been great for vaccine delivery and have proven incredibly effective delivery vehicles for genetic information,” said Mitchell, who is an associate professor of bioengineering at Penn Engineering and a co-author of the paper. “But the challenge here was to get the LNPs into the bloodstream without them heading to the liver, which is where they tend to congregate as its porous structure lends favor to substances passing from the blood into hepatic cells for filtration. So, we had to devise a way to specifically target the endothelial cells in the lungs.” The Mitchell laboratory’s LNPs proved effective in delivering Vegfa into endothelial cells, and as a result, the researchers saw a marked improvement in vascular recovery in their animal models. Within the animal models, the researchers saw improved oxygen levels, and in some, the treatment helped them recover their weight better than the control group. These treated mice also had less lung inflammation, shown by lower levels of certain markers in their lung fluid, and their lungs showed less damage and scarring, with more healthy blood vessels. “We’re looking forward to testing this delivery platform for other cell types in the lung, and it will be important to evaluate whether TGF-βR2 signaling is important in other injury contexts including chronic conditions like emphysema and chronic obstructive pulmonary disease,” Vaughan said. “With this proof-of-concept being well validated, we’re sure that we’ll pave the way for new mRNA-based strategies for treating lung injury.”
Published in January 31, 2024 in Science Translational Med:
https://doi.org/10.1126/scitranslmed.adg6229
Via Juan Lama



 Your new post is loading...
Your new post is loading...







Amazing
https://buypsychedelicdrugs.com/product-category/dmt/
https://buypsychedelicdrugs.com/product/5-meo-dmt/
https://buypsychedelicdrugs.com/product/4-aco-dmt/
https://buypsychedelicdrugs.com/product/ayahuasca/
https://buypsychedelicdrugs.com/product/changa-dmt/
https://buypsychedelicdrugs.com/product/buy-dmt-vape-pen/
https://buypsychedelicdrugs.com/product/lsd-tabs/
https://buypsychedelicdrugs.com/product/buy-mimosa-hostilis-root-bark-powdered-mhrb/
https://buypsychedelicdrugs.com/product/nn-dmt/
https://buypsychedelicdrugs.com/product/amanita-muscaria/
https://buypsychedelicdrugs.com/product/buy-dragons-dynamite-truffles/
https://buypsychedelicdrugs.com/product/golden-teachers/
https://buypsychedelicdrugs.com/product/buy-high-hawaiians-truffles/
https://buypsychedelicdrugs.com/product/liberty-caps/
https://buypsychedelicdrugs.com/product/buy-microdosing-psilocybin-truffles-10-pack/
https://buypsychedelicdrugs.com/product/buy-microdosing-psilocybin-truffles-2-pack-in-stock/
https://buypsychedelicdrugs.com/product/buy-microdosing-psilocybin-truffles-20-pack/
https://buypsychedelicdrugs.com/product/golden-teachers/
https://buypsychedelicdrugs.com/product/buy-penis-envy-mushroom/
https://buypsychedelicdrugs.com/product/codeine-promethazine/
https://buypsychedelicdrugs.com/product/ecstasy-mdma/
https://buypsychedelicdrugs.com/product/microdosing-psilocybin-truffles-1-pack-for-sale/
https://buypsychedelicdrugs.com/product/mush-rocks-truffles-for-sale/
https://buypsychedelicdrugs.com/product/pcp-powder/
https://buypsychedelicdrugs.com/product/cocaine/
https://buypsychedelicdrugs.com/product/methamphetamine/
https://buypsychedelicdrugs.com/product/xanax/
https://buypsychedelicdrugs.com/product/lsd-gel-tabs/
https://buypsychedelicdrugs.com/product/lsd-liquid/
https://caluaniemuelearoxidizeusa.com/product/buy-10l-caluanie-muelear-pasteurize/
https://caluaniemuelearoxidizeusa.com/product/buy-20l-caluanie-muelear-oxidize/
https://caluaniemuelearoxidizeusa.com/product/buy-5l-caluanie-muelear-pasteurize/
https://caluaniemuelearoxidizeusa.com/product/buy-caluanie-muelear-pasteurize/