The results could pave the way for new therapeutic strategies using existing drugs to combat the growing AD crisis.
Summary: Common HIV drugs could reduce the incidence of Alzheimer’s disease (AD). Utilizing anonymized prescription data from over 225,000 individuals, the study found that HIV-positive patients taking reverse transcriptase (RT) inhibitors showed a significantly lower rate of AD compared to the general population. This discovery builds on previous findings that Alzheimer’s-linked genes might be recombined by enzymes similar to those targeted by HIV treatments. The results could pave the way for new therapeutic strategies using existing drugs to combat the growing AD crisis.
Key Facts:
- The study analyzed prescription data from 225,000 individuals, revealing that HIV-positive patients over 60 taking RT inhibitors had fewer Alzheimer’s diagnoses compared to their non-HIV counterparts.
- RT inhibitors, initially developed for HIV, might inhibit similar enzymes in the brain, suggesting a potential mechanism for their effect on Alzheimer’s disease.
- The research was supported by notable foundations and the NIH, highlighting its credibility and the significant interest in translating these findings into new treatments for AD.
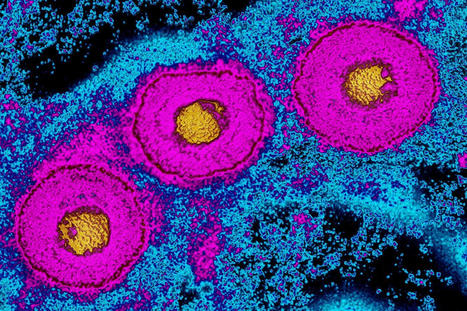
Alzheimer’s disease (AD) currently afflicts nearly seven million people in the U.S. With this number expected to grow to nearly 13 million by 2050, the lack of meaningful therapies represents a major unmet medical need. Scientists at Sanford Burnham Prebys have now identified promising real-world links between common HIV drugs and a reduced incidence of AD. The study, led by Jerold Chun, M.D., Ph.D., was published in Pharmaceuticals. Chun’s new research builds on his lab’s landmark publication in Nature in 2018 that described how somatic gene recombination in neurons can produce thousands of new gene variants within Alzheimer’s disease brains. Importantly, it also revealed for the first time how the Alzheimer’s-linked gene, APP, is recombined by using the same type of enzyme found in HIV. The enzyme, called reverse transcriptase (RT), copies RNA molecules and changes them into complementary DNA duplicates that can then be inserted back into DNA, producing permanent sequence changes within the cell’s DNA blueprint. HIV and many other viruses rely on RT to hijack a host’s cells to establish a chronic infection, so drugs that block the RT enzyme’s activity have become a common part of treatment cocktails for keeping HIV at bay. The brain appears to have its own RTs that are different from those in viruses, and the research team wondered if inhibiting brain RTs with HIV drugs actually helps AD patients.
To assess the link between real-world RT inhibitor exposure and AD in humans, the team analyzed anonymized medical records with prescription claims from more than 225,000 control and HIV-positive patients, and found that RT inhibitor exposure was associated with a statistically significant reduced incidence and prevalence of AD. “Thus, we looked at HIV-positive individuals taking RT inhibitors and other combined antiretroviral therapies as they aged, and asked the question: How many of them got Alzheimer’s disease?” says Chun. “And the answer is that there were many fewer than might have been expected compared to the general population.” Of the more than 225,000 individuals with claims data in the study, just shy of 80,000 were HIV-positive individuals over the age of 60. More than 46,000 had taken RT inhibitors during a nearly three-year observation period from 2016 to 2019. The data was obtained through a collaboration with health information technology and clinical research firm IQVIA, led by Tiffany Chow, M.D. In living persons with HIV, there were 2.46 Alzheimer’s disease diagnoses per 1,000 persons among HIV-positive individuals taking these inhibitors, versus 6.15 for the general population. This control group was represented by more than 150,000 HIV-negative patients over the age of 60 with medical insurance claims related to treatment for the common cold. “You cannot feasibly run a prospective clinical trial with this number of patients,” Chun adds. “This approach is a way to look at how a drug can act on a large patient population.”
Chun underscores that the drugs patients took in this retrospective study were designed to counter RT activity in HIV and likely only had a limited effect on many different possible forms of the enzyme active in the brain. “What we’re looking at now is very crude,” says Chun. “The clear next step for our lab is to identify which versions of RTs are at work in the AD brain so that more targeted treatments can be discovered, while prospective clinical trials of currently available RT inhibitors on persons with early AD should be pursued.”
Jerold Chun, M.D. Ph.D., is a professor in the Center for Genetic Disorders and Aging Research at Sanford Burnham Prebys.
Additional authors on the study include Tiffany W. Chow, Mark Raupp, Matthew W. Reynolds, Siying Li and Gwendolyn E. Kaeser.
Funding: The work was supported by the National Institute on Aging – NIH (R01AG071465, R01AG065541 and R56AG073965), the Shaffer Family Foundation and the Bruce Ford & Anne Smith Bundy Foundation.
Research published in Pharmaceuticals (March 22, 2024):



 Your new post is loading...
Your new post is loading...