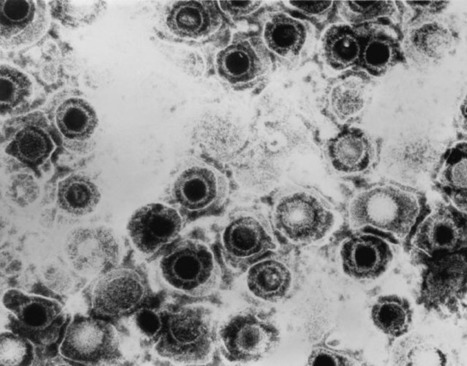
Three cell-based models shed light on how herpes simplex virus type 1 (HSV-1) infection, which can spread to the fetal brain during pregnancy, may contribute to various neurodevelopmental disabilities and long-term neurological problems into adulthood, according to a study published October 22, 2020 in the open-access journal PLOS Pathogens by Pu Chen and Ying Wu of Wuhan University, and colleagues. HSV-1 is a highly prevalent pathogen that can cause lifelong neurological problems such as cognitive dysfunction, learning disabilities, and dementia. But progress in understanding the role of HSV-1 in human fetal brain development has been hampered by restricted access to fetal human brain tissue as well as limitations of existing animal models. To address this gap in knowledge, the researchers generated three different cell-based neurodevelopmental disorder models, including a 2-D layer of cells and a 3-D brain-like structure. These models are based on human induced pluripotent stem cells (hiPSCs) - immature, embryonic stem cell-like cells that are generated by genetically reprogramming specialized adult cells.
HSV-1 infection in neural stem cells derived from hiPSCs resulted in activation of the caspase-3 apoptotic pathway, which initiates programmed cell death. HSV-1 infection also impaired the production of new neurons, and hindered the ability of hiPSC-derived neural stem cells to convert into mature neurons through a process called neuronal differentiation. Moreover, the HSV-1-infected brain organoids mimicked the pathological features of neurodevelopmental disorders in the human fetal brain, including impaired neuronal differentiation and abnormalities in brain structure. In addition, the 3-D model showed that HSV-1 infection promotes the abnormal proliferation and activation of non-neuronal cells called microglia, accompanied by the activation of inflammatory molecules, such as TNF-α, IL-6, IL-10, and IL-4. According to the authors, the findings open new therapeutic avenues for targeting viral reservoirs relevant to neurodevelopmental disorders. The authors add, "This study provides novel evidence that HSV-1 infection impaired human brain development and contributed to the neurodevelopmental disorder pathogen hypothesis".
Original study published in PLOS Pathogens (Oct. 22):



 Your new post is loading...
Your new post is loading...