Your new post is loading...

|
Scooped by
Juan Lama
|
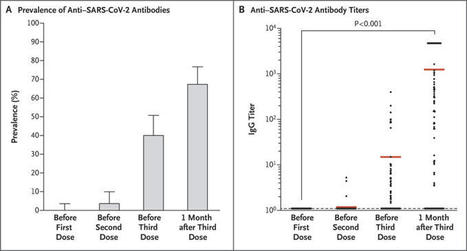
A weak immune response to two doses of vaccine against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has been observed in recipients of solid-organ transplants.1,2 Severe cases of coronavirus disease 2019 (Covid-19) have also been reported in transplant recipients who had received two doses of vaccine.3 These reports prompted the French National Authority for Health to recommend the use of a third dose in immunosuppressed patients.4 Here, we report the humoral response in a group of 101 consecutive solid-organ transplant recipients (mean [±SD] age, 58±2 years; 69% were men) who were given three doses of the messenger RNA vaccine BNT162b2 (Pfizer–BioNTech). The group included 78 kidney-transplant recipients, 12 liver-transplant recipients, 8 lung-transplant or heart-transplant recipients, and 3 pancreas-transplant recipients. The first two doses were given 1 month apart, and the third dose was administered 61±1 days after the second dose. The time between transplantation and the initiation of vaccination was 97±8 months. Immunosuppression was due to the use of glucocorticoids (in 87% of patients), calcineurin inhibitors (in 79% of patients), mycophenolic acid (in 63% of patients), mammalian target of rapamycin inhibitors (in 30% of patients), and belatacept (in 12% of patients). The levels of antibodies to SARS-CoV-2 spike protein were assessed in all the patients with the use of the Wantai enzyme-linked immunosorbent assay (Beijing Wantai Biological Pharmacy Enterprise).5 Antibody titers are expressed as the ratio of the sample signal to a calibrator-assigned cutoff signal (the signal-to-cutoff ratio). According to French law, because this was an anonymous retrospective study, institutional review board approval was not required. The prevalence of anti–SARS-CoV-2 antibodies was 0% (95% confidence interval [CI], 0 to 4; 0 of 101 patients) before the first dose, 4% (95% CI, 1 to 10; 4 of 101 patients) before the second dose, 40% (95% CI, 31 to 51; 40 of 99 patients) before the third dose, and 68% (95% CI, 58 to 77; 67 of 99 patients) 4 weeks after the third dose (Figure 1). Among the 59 patients who had been seronegative before the third dose, 26 (44%) were seropositive at 4 weeks after the third dose (mean [±SD] signal-to-cutoff ratio, 690±293). All 40 patients who had been seropositive before the third dose were still seropositive 4 weeks later; their antibody titers increased from 36±12 before the third dose to 2676±350 1 month after the third dose (P<0.001). Patients who did not have an antibody response were older, had a higher degree of immunosuppression, and had a lower estimated glomerular filtration rate than patients who had an antibody response (see the Supplementary Appendix, available with the full text of this letter at NEJM.org). As of this writing, Covid-19 had not developed in any of the patients after they received the three vaccine doses. No serious adverse events were reported after the administration of the third dose, and no acute rejection episodes occurred. This study showed that administration of a third dose of the BNT162b2 vaccine to solid-organ transplant recipients significantly improved the immunogenicity of the vaccine, with no cases of Covid-19 reported in any of the patients. However, a large proportion of the patients remain at risk for Covid-19. Barrier measures should be maintained, and vaccination of the relatives of these patients should be encouraged. Published in NEJM (June 23, 2021): https://doi.org/10.1056/NEJMc2108861

|
Scooped by
Juan Lama
|
Dengue infection (DI) is the most important arboviral infection in the world. The majority of immunocompetent patients will have asymptomatic or mild infections, but the degree of dengue severity in kidney transplant recipients (KTx) is unknown. In recent decades, the growing number of organ transplant recipients in developing countries, living in or traveling to an endemic area of dengue, is at risk of developing this infection. Additionally, in kidney transplant recipients (KTx), DI may be associated with other viral infections, such as cytomegalovirus (CMV), increasing the risk for the recipients after renal transplantation (Tx). Because CMV remains one of the most important viruses affecting KTx, it is not clear whether the CMV coinfection may modify the outcome of DI as it usually does in other viral coinfections In this study, we report the clinical profile and outcomes of 39 dengue cases in KTx. From a total of 1,186 KTx outpatients in follow-up we reviewed clinical and laboratory records of 60 (5%) patients admitted with suspected DI initially screened by NS-1, IgM, and when possible, multiplex nested PCR. The prevalence of DI in KTx was 3% (39/1,118), with symptoms leading to hospital admission being fever, myalgia, malaise, and headache. Laboratory tests showed leucopenia, thrombocytopenia, and liver enzyme elevation. DI was confirmed by positivity of NS-1 (33%), IgM (69%), and/or RT-PCR (59%). Twenty-three patients (59%) had dengue with warning signs, and 15% had severe dengue, 2 of them with a fatal course. Acute graft dysfunction occurred in 59% (mean nadir serum creatinine: 2.9 ± 2.6mg/dL), 4 of them requiring dialysis. CMV coinfection diagnosed in 19% of the cases and patients was associated with worse clinical presentation. Our results suggest that KTx with DI presented initial physical and laboratorial profile similar to the general population. However, DI in KTx seems to have a higher risk for graft dysfunction, severe dengue, and death. Because CMV coinfection aggravates the DI clinical presentation and recovery, it must be evaluated in all cases. Published in PLOS One (October 30, 2019): https://doi.org/10.1371/journal.pone.0219117

|
Scooped by
Juan Lama
|
For the first time in Southern California, surgeons at UC San Diego Health have transplanted the kidney of a deceased donor with HIV into a recipient with a pre-existing HIV infection. The procedure is part of an unprecedented multi-site national clinical trial. The procedure occurred earlier this month. The patient is expected to make a full recovery. In 2013, Congress passed the HIV Organ Policy Equity (HOPE) Act, an effort to alleviate a chronic shortage of donor organs, which hits patients with HIV particularly hard, resulting in extremely long wait times and a greater likelihood of dying before a donor organ becomes available. Though organ transplants between donors and recipients with HIV have been successfully conducted in South Africa since 2008, such transplants were illegal in the U.S. until passage of the HOPE Act, which permits transplants of kidneys and livers from donors with HIV to qualified recipients with well-controlled HIV and end-stage organ failure, under approved research protocols. The kidney clinical trial launched last year. The transplantation of organs from donors with HIV to recipients without HIV remains prohibited. The shortage of donor organs is universal and persistent, with more than 113,000 Americans currently needing a transplant (with almost 75,000 on active waiting lists), according to the United Network for Organ Sharing. The kidney was the first human organ to be successfully transplanted in 1954 and is, by far, the organ most often transplanted. The use of donor organs infected with HIV or hepatitis B and C viruses has become more viable in recent years. In 2016, Saima Aslam, MBBS, associate professor of medicine at UC San Diego School of Medicine and director of the Solid Organ Transplant Infectious Diseases Service at UC San Diego Health, and colleagues in the organ transplant programs launched a clinical practice protocol to use organs from donors actively infected with the hepatitis C virus, which is now curable. The change has resulted in a significant expansion of the organ donor pool and a reduction in wait list time. Persons with HIV are at higher risk of requiring a kidney (or liver) transplant due to organ damage caused by the virus and by common, associated co-infections and conditions, such as hepatitis B and C, hypertension and diabetes. UC San Diego is also participating in a second, similar clinical trial involving HIV-to-HIV liver transplants. That first-ever trial launched earlier this year at UC San Diego; it is actively recruiting patients as well.
|

|
Scooped by
Juan Lama
|
While all participants in the control group displayed a positive antibody response to spike protein, only 51 of the 136 (37.5%) organ transplant recipients had positive serology. Researchers have found that organ transplant recipients may remain at high risk for COVID-19 even after being fully vaccinated against the novel coronavirus. The Israeli study analyzed the humoral responses of 139 kidney transplant recipients after receiving both shots of the Pfizer-BioNTech vaccine, benchmarking their results against a control group of 25 healthy participants. Across the board, the mean antibody levels "were significantly lower" in comparison to the control participants, the researchers said. Transplant recipients who did in fact display a positive serology were typically younger than those without. Additionally, the longer period of time between transplantation and vaccination was "significantly associated" with positive serological response to mRNA vaccines. "The most significant predictors of failure to mount a humoral response in our cohort of kidney transplant recipients were advanced age, need for high dose corticosteroids during the last (pre-vaccination) year, maintenance with three immunosuppressive medications, and a regimen that includes [Mycophenolate mofetil] MMF," the study authors wrote. Researchers added that MMF is known to have a "suppressive effect on the immune system, including inhibition of antibody production," noting that "the greater the degree of immunosuppression, the less likely the patient will respond to immunization." Out of the 139 study participants, only two developed severe COVID-19 infections following a full vaccination. One required severe hospitalization 12 weeks after being vaccinated, and the other died, nine weeks after receiving the second dose of the Pfizer vaccine. The reduced response rates to vaccinations among transplant recipients have been well documented throughout previously published studies covering other common vaccines such as those that protect against hepatitis B, the flu or pneumococcal ones. While the study confirms previous findings, the researchers note that further research needs to be done to figure out whether or not patients with these low serological levels are at a higher risk of contracting coronavirus, and what the severity of the sickness would be if so, considering there has not been a well-established "protective antibodies threshold." Researchers recommend that organ transplant recipients be counseled regarding their own personal immunization, and take an "individual approach" to the matter, in addition to continuing to practice social distancing and other measures to protect themselves against COVID-19 infections. Original findings published in the American Journal of Transplantation (April 18, 2021): See also vaccines effect on lung transplant recipients (May 5, 2021):

|
Scooped by
Juan Lama
|
People infected with hepatitis C may be able to donate their kidney without the risk of infection spreading, a study has suggested. Hepatitis C is spreads through the bloodstream, therefore those infected are not allowed to donate blood or organs. Currently, hepatitis C kidneys can only be transferred to patients already infected with the virus. But American scientists now say the process is safe after successfully transplanting 53 infected kidneys into healthy recipients, none of whom contracted the virus. American scientists say transplanting kidneys from patients with hepatitis C is safe after successfully transplanting 53 infected kidneys into healthy recipients. Hepatitis C is a viral infection that inflames the liver and is usually acquired from infected blood. If left untreated, the infection can cirrhosis - or scarring of the liver. Over time, this can cause the liver to stop working properly. In severe cases, life-threatening problems such as liver failure or liver cancer can eventually develop. The virus killed 1.34million people in 2016 alone - 140,000 more than tuberculosis, 340,000 more than HIV and 621,00 more than malaria. Worldwide, it affects 71million people, and a great number of those infected will develop liver cancer or cirrhosis in the future. The study was carried out by the University of Tennessee Health Science Centre in Memphis. All kidneys were successfully transplanted and participants received a 12-week-long antiviral therapy. None of the patients showed any signs of hepatitis C following the procedures but they did contract other viral infections. Three developed the BK virus, which is common after transplantation and is treatable. Symptoms can feel like a common cold. The BK virus is a latent infection that lives in the kidneys in about 90 per cent of healthy people who show no sign of infection. Reactivation can occur after an organ transplant as the the immune system is put under heightened stress. But by the end of the 12-week study, all participants were infection-free. Results of the trial were published in July 15, 2019 in American Journal of Transplantation:
|



 Your new post is loading...
Your new post is loading...