Your new post is loading...

|
Scooped by
Juan Lama
|
One of the major challenges currently faced by global health systems is the prolonged COVID-19 syndrome (also known as “long COVID”) which has emerged as a consequence of the SARS-CoV-2 epidemic. It is estimated that at least 30% of patients who have had COVID-19 will develop long COVID. In this study, our goal was to assess the plasma metabolome in a total of 100 samples collected from healthy controls, COVID-19 patients, and long COVID patients recruited in Mexico between 2020 and 2022. A targeted metabolomics approach using a combination of LC–MS/MS and FIA MS/MS was performed to quantify 108 metabolites. IL-17 and leptin were measured in long COVID patients by immunoenzymatic assay. The comparison of paired COVID-19/long COVID-19 samples revealed 53 metabolites that were statistically different. Compared to controls, 27 metabolites remained dysregulated even after two years. Post-COVID-19 patients displayed a heterogeneous metabolic profile. Lactic acid, lactate/pyruvate ratio, ornithine/citrulline ratio, and arginine were identified as the most relevant metabolites for distinguishing patients with more complicated long COVID evolution. Additionally, IL-17 levels were significantly increased in these patients. Mitochondrial dysfunction, redox state imbalance, impaired energy metabolism, and chronic immune dysregulation are likely to be the main hallmarks of long COVID even two years after acute COVID-19 infection. Published in Scientific Reports (August 1, 2023): https://doi.org/10.1038/s41598-023-39049-x

|
Scooped by
Juan Lama
|
Two-thirds of those in the study sought medical care a month to six months afterward, and about two-thirds of those who sought care were found to have an entirely new medical condition. Most adults who test positive for the coronavirus don’t require hospitalization but tend to seek medical care in subsequent months, and two-thirds of those who do are told they have a health condition they did not have before. These are the findings of a study conducted by investigators from the Centers for Disease Control and Prevention and Kaiser Permanente, which included some 3,171 members of the Kaiser Permanente Georgia integrated health care system. More than half were Black. The message for patients is that even for those who have had only mild Covid-19, “it’s possible you may experience new or persistent symptoms months after the initial diagnosis,” said Dr. Alfonso C. Hernandez-Romieu, an infectious disease specialist with the C.D.C., and the study’s lead author. “And it’s important for people to make sure they’re going to their clinicians,” he said, to express their concerns. “It’s equally important,” he added, “for clinicians to acknowledge that there may be these long-term effects and to really make sure they’re validating patients, treating them with empathy and trying to help them in the best way possible.” Clinicians need to monitor patients for Covid-19-related complications that are potentially very serious, like blood clots, he said. The study did not compare patients who tested positive for the coronavirus to patients who did not, so the authors were unable to say whether people who had recovered from mild Covid-19 cases made more doctors’ visits than those who never had the virus. But two-thirds of the patients who had mild disease sought medical care one to six months after their Covid-19 diagnoses, and about two-thirds of those who sought care were found to have an entirely new condition. The new diagnoses included cough, shortness of breath, heart rate abnormalities, chest or throat pain, and fatigue, “which likely represent ongoing Covid-19 symptoms,” the study said. Among those more likely to seek medical care were adults 50 and older, women and those with underlying health conditions. Black adults were also slightly more likely than others to seek care. But over all, the authors noted, the number of visits declined over time. The potential for long-term complications, even after a mild course of disease, underscores the need for prevention measures and vaccination, Dr. Hernandez-Romieu said. “There is a lot we don’t know about post-Covid conditions,” he said. “Even though a majority of people don’t end up with severe Covid, or end up in the hospital, the potential for long-term health effects is really important.” Cited study published in MMWR (April 23, 2021): http://dx.doi.org/10.15585/mmwr.mm7017e3

|
Scooped by
Juan Lama
|
Using cardiac MRI, researchers found myocardial injury in more than half of patients hospitalized with severe COVID-19 and elevated troponin a few months after hospital discharge. “We found evidence of high rates of heart muscle injury that could be seen on the scans a month or two after discharge. Whilst some of this may have been preexisting, MRI scanning shows that some were new, and likely caused by COVID-19,” Marianna Fontana, MD, PhD, professor of cardiology at University College London, said in a press release. “Importantly, the pattern of damage to the heart was variable, suggesting that the heart is at risk of different types of injury. While we detected only a small amount of ongoing injury, we saw injury to the heart that was present even when the heart’s pumping function was not impaired and might not have been picked up by other techniques. In the most severe cases, there are concerns that this injury may increase the risks of heart failure in the future, but more work is needed to investigate this further.” For this analysis, researchers included 148 patients from six hospitals (mean age, 64 years; 70% men) with severe COVID-19 infection and elevated troponin levels, all requiring hospitalization (32% requiring mechanical ventilation), who underwent convalescent cardiac MRI and adenosine stress perfusion at a median of 68 days after discharge. “Raised troponin levels are associated with worse outcomes in COVID-19 patients. Patients with severe COVID-19 disease often have preexisting heart-related health problems, including diabetes, raised blood pressure and obesity,” Fontana said in the release. “During severe COVID-19 infection, however, the heart may also be directly affected. Unpacking how the heart can become damaged is difficult, but MRI scans of the heart can identify different patterns of injury, which may enable us to make more accurate diagnoses and to target treatments more effectively.” Myocardial injury in COVID-19 Patients with abnormal troponin levels were offered a cardiac MRI after discharge and were compared with a control group of patients who did not have COVID-19 and 40 healthy volunteers. Researchers observed that left ventricular function was normal in 89% of the overall cohort (mean ejection fraction, 67%). Late gadolinium enhancement and/or ischemia was found in 54% of participants hospitalized for severe COVID-19 infection, which included a myocarditis-like scar in 26%, MI and/or ischemia in 22% and dual pathology in 6%. According to the study, myocarditis-like injury was limited to three or fewer myocardial segments in 88% of patients with no LV dysfunction, of which 30% had active myocarditis. In addition, MI was observed in 19% and inducible ischemia in 26% of patients who underwent stress perfusion after discharge. Moreover, of patients with ischemic injury, 66% had no prior history of coronary disease. Researchers found no evidence of diffuse fibrosis or edema in the remote myocardium. Two new opportunities “These findings give us two opportunities,” Fontana said in the release. “Firstly, to find ways of preventing the injury in the first place, and from some of the patterns we have seen, blood clotting may be playing a role, for which we have potential treatments. Secondly, detecting the consequences of injury during convalescence may identify subjects who would benefit from specific supporting drug treatments to protect heart function over time.” Findings published in European Heart Journal (Feb. 18, 2021): https://doi.org/10.1093/eurheartj/ehab075

|
Scooped by
Juan Lama
|
By early January, 2021, COVID-19, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), had resulted in more than 83 million confirmed cases and more than 1·8 million deaths. The clinical spectrum of SARS-CoV-2 infection is wide, encompassing asymptomatic infection, fever, fatigue, myalgias, mild upper respiratory tract illness, severe life-threatening viral pneumonia requiring admission to hospital, and death. Physicians are observing persisting symptoms and unexpected, substantial organ dysfunction after SARS-CoV-2 infection in an increasing number of patients who have recovered, as previously observed in the SARS outbreak. However, COVID-19 is a new disease and uncertainty remains regarding the possible long-term health sequelae. This is particularly relevant for patients with severe symptoms, including those who required mechanical ventilation during their hospital stay, for whom long-term complications and incomplete recovery after discharge would be expected. Unfortunately, few reports exist on the clinical picture of the aftermath of COVID-19. The study by Chaolin Huang and colleagues in The Lancet is relevant and timely. They describe the clinical follow-up of a cohort of 1733 adult patients (48% women, 52% men; median age 57·0 years, IQR 47·0–65·0) with COVID-19 who were discharged from Jin Yin-tan Hospital (Wuhan, China). 6 months after illness onset, 76% (1265 of 1655) of the patients reported at least one symptom that persisted, with fatigue or muscle weakness being the most frequently reported symptom (63%, 1038 of 1655). More than 50% of patients presented with residual chest imaging abnormalities. Disease severity during the acute phase was independently associated with the extent of lung diffusion impairment at follow-up (odds ratio 4·60, 95% CI 1·85–11·48), with 56% (48 of 86) of patients requiring high-flow nasal cannula, non-invasive ventilation, and invasive mechanical ventilation during their hospital stay having impaired pulmonary diffusion capacity. These findings are consistent with those from earlier small studies that reported lingering radiological and pulmonary diffusion abnormalities in a sizeable proportion of COVID-19 patients up to 3 months after hospital discharge. Evidence from previous coronavirus outbreaks suggests that some degree of lung damage could persist, as shown in patients who recovered from SARS, 38% of whom had reduced lung diffusion capacity 15 years after infection. Although SARS-CoV-2 primarily affects the lungs, several other organs, including the kidney, can also be affected. Therefore, Huang and colleagues assessed the sequelae of extrapulmonary manifestations of COVID-19. Unexpectedly, 13% (107 of 822) of the patients who did not develop acute kidney injury during their hospital stay and presented with normal renal function, based on estimated glomerular filtration rate (eGFR) during the acute phase, exhibited a decline in eGFR (<90 mL/min per 1·73 m2) at follow-up. However, this finding must be interpreted with caution... Original findings published in the Lancet (Jan. 8, 2021):
|

|
Scooped by
Juan Lama
|
Long-haul COVID-19 patients face many health threats -- including a higher chance of dying -- up to 6 months after they catch the virus, according to a massive study published in the journal Nature. A second study, released by the CDC on Friday, also found lingering symptoms months later among COVID-19 patients who originally had mild symptoms. For the Nature study, researchers examined more than 87,000 COVID-19 patients and nearly 5 million control patients in a federal database. They found COVID-19 patients had a 59% higher risk of death up to 6 months after infection, compared to non-infected people. Those findings translate into about eight extra deaths per 1,000 patients over 6 months, because many deaths caused by long-term COVID complications are not recorded as COVID-19 deaths, the researchers said. Among patients who were hospitalized and died after more than 30 days, there were 29 excess deaths per 1,000 patients over 6 months. “As far as total pandemic death toll, these numbers suggest that the deaths we’re counting due to the immediate viral infection are only the tip of the iceberg,” Ziyad Al-Aly, MD, the senior author of the study and a director of the Clinical Epidemiology Center at the Veterans Affairs St. Louis Health Care System, said in a news release from the University of Washington Medical School in St. Louis. Johns Hopkins University says more than 3 million people worldwide and about 570,000 people in the United States have died of coronavirus-related reasons. Long-haul COVID patients also had a much higher chance of getting sick, and not just in the respiratory system, according to the study. The patients had a high rate of stroke and other nervous system ailments; mental health problems such as depression; the onset of diabetes; heart disease and other coronary problems; diarrhea and digestive disorders; kidney disease; blood clots; joint pain; hair loss; and general fatigue. Patients often had clusters of these ailments. And the more severe the case of COVID-19, the higher the chance of long-term health problems, the study said. Researchers based their study on health care databases of the U.S. Department of Veterans Affairs. Besides the 87,000 COVID patients, the database included about 5 million patients who didn’t catch COVID. The veterans in the study were about 88% men, but the large sample size included 8,880 women with confirmed cases, the news release said. Al-Aly, an assistant professor at Washington University Medical School, said the study shows that long-haul COVID-19 could be “America’s next big health crisis.” “Our study demonstrates that up to 6 months after diagnosis, the risk of death following even a mild case of COVID-19 is not trivial and increases with disease severity,” he said. “Given that more than 30 million Americans have been infected with this virus, and given that the burden of long COVID-19 is substantial, the lingering effects of this disease will reverberate for many years and even decades.” Meanwhile, the CDC on Friday released a new study of people who had milder cases of COVID-19. It found that almost two-thirds of them returned to the doctor within 6 months of their initial infections with new symptoms. The study validates the accounts of many COVID-19 long haulers who say they are still sick months later though their initial infections were mild. More than 3,100 cases were reviewed for the study. None of the patients had been hospitalized for their initial infections. The study found that nearly 70%, or 2,100 people, with mild infections treated by the Kaiser Permanente health system in Georgia returned to the doctor 1 to 6 months after that initial diagnosis, and nearly 40% needed to see a specialist. Compared to people who didn’t return to the doctor after recovering from their initial infections, the long haulers were more likely to be African American, women, and people over the age of 50. About 10% of them were given a second diagnosis of an active COVID infection. “Health care providers used the diagnosis of active infection to indicate that the effects of COVID-19 were affecting medical care at the time of the visit,” study author Alfonso Hernandez-Romieu, MD, said in an email. “Therefore it cannot be determined whether patients might have been experiencing symptoms of reinfection with SARS-CoV-2, rather than ongoing COVID-19 symptoms,” said Hernandez-Romieu, who is part of the clinical team at CDC studying the long-term complications of COVID-19. Pulmonologists, cardiologists, neurologists, and mental health professionals were some of the most frequently consulted specialties. The study authors say doctors should be aware that patients coming to them might have new symptoms related to a past COVID diagnosis. See also publication in Nature (April 22, 2021): https://doi.org/10.1038/s41586-021-03553-9 Publication in MMWR (April 23, 2021): http://dx.doi.org/10.15585/mmwr.mm7017e3

|
Scooped by
Juan Lama
|
An analysis of electronic medical records in California found that 32 percent started with asymptomatic infections but reported troubling aftereffects weeks and months later. The study, one of the first to focus exclusively on people who never needed to be hospitalized when they were infected, analyzed electronic medical records of 1,407 people in California who tested positive for the coronavirus. More than 60 days after their infection, 27 percent, or 382 people, were struggling with post-Covid symptoms like shortness of breath, chest pain, cough or abdominal pain. Nearly a third of the patients with such long-term problems had not had any symptoms from their initial coronavirus infection through the 10 days after they tested positive, the researchers found. Understanding long-term Covid symptoms is an increasingly pressing priority for doctors and researchers as more and more people report debilitating or painful aftereffects that hamper their ability to work or function the way they did before. Last month, the director of the National Institutes of Health, Dr. Francis S. Collins, announced a major initiative “to identify the causes and ultimately the means of prevention and treatment of individuals who have been sickened by Covid-19, but don’t recover fully over a period of a few weeks.” David Putrino, director of rehabilitation innovation at Mount Sinai Health System in New York City, who was not involved in the new research, said that he and his colleagues at Mount Sinai’s center for post-Covid care are seeing a similar pattern. “Many people who had asymptomatic Covid can also go on to develop post-acute Covid syndrome,” said Dr. Putrino, who is a co-author of a smaller study on the topic published last year. “It doesn’t always match up with severity of acute symptoms, so you can have no symptoms but still have a very aggressive immune response.” The new study is published on the preprint site MedRxiv and has not finished undergoing peer review. Its strengths include that it is larger than many studies on long-term symptoms published so far and that the researchers used electronic records from the University of California system, allowing them to obtain health and demographic information of patients from throughout the state. The researchers also excluded from the study symptoms that patients had reported in the year before their infection, a step intended to ensure a focus on post-Covid symptoms. Among their findings: Long-term problems affect every age group, including children. “Of the 34 children in the study, 11 were long-haulers,” said one of the authors, Melissa Pinto, an associate professor of nursing at the University of California Irvine. The study found more than 30 symptoms, including anxiety, low back pain, fatigue, insomnia, gastrointestinal problems and rapid heart rate. The researchers identified five clusters of symptoms that seemed most likely to occur together, like chest pain and cough or abdominal pain and headache. Most previous studies of long-term symptoms have tended to involve people who were sick enough from their initial infection to be hospitalized. One of the largest found that more than three-quarters of about 1,700 hospitalized patients in Wuhan, China, had at least one symptom six months later. But increasingly, people who were never hospitalized are seeking care at post-Covid clinics, and scientists are recognizing the need to understand their circumstances. Last month, researchers at the University of Washington reported on a survey of 177 people who had tested positive for the coronavirus. Most of them had not been hospitalized. About a third of both the people who had been hospitalized and the people who had only mild initial illnesses reported having at least one lasting symptom six months later, the researchers found. Unlike some recent surveys, like one by a patient-led research team, the new study did not capture one of the most commonly reported “long Covid” issues: cognitive problems like brain fog, memory problems and difficult concentrating. One of the co-authors, Natalie Lambert, an associate research professor at Indiana University School of Medicine, said that may be because at the time, doctors may not have known to include diagnostic codes for such cognitive issues in the medical records of Covid patients. The team is seeking funding for a larger and more comprehensive study that combines information in medical records, doctors’ notes and patients’ reports, she said. In the new study, about 59 percent of the patients with long-term symptoms were women, and about half of the patients were Hispanic and 31 percent were white. The authors and Dr. Putrino cautioned that any reliable demographic conclusions would require bigger studies that are national in scope. Dr. Lambert said it was likely that the medical records used in the study reflected only a percentage of people who had asymptomatic Covid infections and experienced Covid aftereffects. “For some people, if they’re asymptomatic and they don’t know that they’re sick, they’re not going to go get tested,” she said. “Another important component is that we know that some of the long-haul symptoms show up much later than two months,” Dr. Lambert said. “So there’s a potential for a wide range of long-haul symptoms that they’re not going to associate with Covid.” Dr. Pinto said it would be important to study the condition over time, instead of in a static snapshot. “The long haul is a very dynamic process and symptoms can change from day to day,” she said. “One day they may have chest pain and a headache, and the very next day, the chest pain and headache is gone and they have backache and muscle aches. We need to capture trajectory and changing of symptoms across time, and we need this in a larger sample that represents America.” Cited study poosted in medRxiv (March 5, 2021): https://doi.org/10.1101/2021.03.03.21252086

|
Scooped by
Juan Lama
|
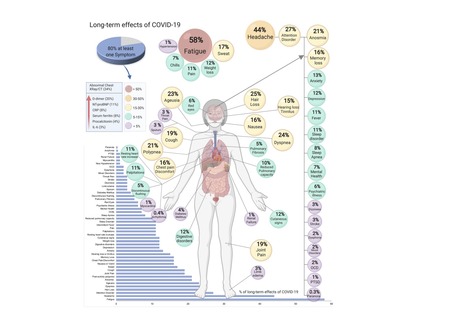
COVID-19, caused by SARS-CoV-2, can involve sequelae and other medical complications that last weeks to months after initial recovery, which has come to be called Long-COVID or COVID long-haulers. This systematic review and meta-analysis aims to identify studies assessing long-term effects of COVID-19 and estimates the prevalence of each symptom, sign, or laboratory parameter of patients at a post-COVID-19 stage. LitCOVID (PubMed and Medline) and Embase were searched by two independent researchers. All articles with original data for detecting long-term COVID-19 published before 1st of January 2021 and with a minimum of 100 patients were included. For effects reported in two or more studies, meta-analyses using a random-effects model were performed using the MetaXL software to estimate the pooled prevalence with 95% CI. Heterogeneity was assessed using I2 statistics. The Preferred Reporting Items for Systematic Reviewers and Meta-analysis (PRISMA) reporting guideline was followed. A total of 18,251 publications were identified, of which 15 met the inclusion criteria. The prevalence of 55 long-term effects was estimated, 21 meta-analyses were performed, and 47,910 patients were included. The follow-up time ranged from 15 to 110 days post-viral infection. The age of the study participants ranged between 17 and 87 years. It was estimated that 80% (95% CI 65-92) of the patients that were infected with SARS-CoV-2 developed one or more long-term symptoms. The five most common symptoms were fatigue (58%), headache (44%), attention disorder (27%), hair loss (25%), and dyspnea (24%). All meta-analyses showed medium (n=2) to high heterogeneity (n=13). In order to have a better understanding, future studies need to stratify by sex, age, previous comorbidities, severity of COVID-19 (ranging from asymptomatic to severe), and duration of each symptom. From the clinical perspective, multi-disciplinary teams are crucial to developing preventive measures, rehabilitation techniques, and clinical management strategies with whole-patient perspectives designed to address long COVID-19 care. Preprint available in medRxiv (Jan. 30, 2021): https://doi.org/10.1101/2021.01.27.21250617
|



 Your new post is loading...
Your new post is loading...