Your new post is loading...

|
Scooped by
Juan Lama
|
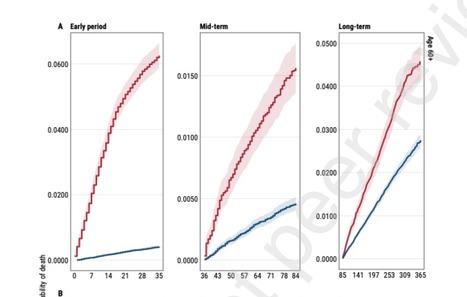
Background: The objective of this study was to describe 12-month mortality following COVID-19 compared with a reference population with no history of COVID-19.
Methods: Retrospective nationwide cohort study using electronic health care data on cases (n= 66,287 COVID-19 patients) and controls (n=254,969) with linkage to SARS-CoV-2 testing and death records.
Results: People infected with COVID-19 had more than three times the risk of dying over the following year compared with those who remained uninfected. Short-term mortality (up to 5 weeks post-infection) was significantly higher among COVID-19 patients (1623/10 000) than controls (118/10 000). For COVID-19 cases over 60 years old, increased mortality persisted until the end of the first year after infection, and was related to increased risk for cardiovascular (aHR 2·1, 95%CI 1·8-2·3), cancer (aHR 1·5, 95%CI 1·2-1·9), respiratory system diseases (aHR 1·9, 95%CI 1·2-3·0), and other causes of death (aHR 1·8, 95%CI 1·4-2·2).
Conclusions: Increased risk of death from COVID-19 is not limited to the acute illness· COVID-19 infection carries a substantially increased risk of death in the following 12 months. This excess death mainly occurs in older people and is driven by broad array of causes of death. Preprint available (The Lancet, Feb. 7, 2022): https://papers.ssrn.com/sol3/papers.cfm?abstract_id=4028547

|
Scooped by
Juan Lama
|
Aims Long-term sequelae may occur after SARS-CoV-2 infection. We comprehensively assessed organ-specific functions in individuals after mild to moderate SARS-CoV-2 infection compared with controls from the general population. Methods and results Four hundred and forty-three mainly non-hospitalized individuals were examined in median 9.6 months after the first positive SARS-CoV-2 test and matched for age, sex, and education with 1328 controls from a population-based German cohort. We assessed pulmonary, cardiac, vascular, renal, and neurological status, as well as patient-related outcomes. Bodyplethysmography documented mildly lower total lung volume (regression coefficient −3.24, adjusted P = 0.014) and higher specific airway resistance (regression coefficient 8.11, adjusted P = 0.001) after SARS-CoV-2 infection. Cardiac assessment revealed slightly lower measures of left (regression coefficient for left ventricular ejection fraction on transthoracic echocardiography −0.93, adjusted P = 0.015) and right ventricular function and higher concentrations of cardiac biomarkers (factor 1.14 for high-sensitivity troponin, 1.41 for N-terminal pro-B-type natriuretic peptide, adjusted P ≤ 0.01) in post-SARS-CoV-2 patients compared with matched controls, but no significant differences in cardiac magnetic resonance imaging findings. Sonographically non-compressible femoral veins, suggesting deep vein thrombosis, were substantially more frequent after SARS-CoV-2 infection (odds ratio 2.68, adjusted P < 0.001). Glomerular filtration rate (regression coefficient −2.35, adjusted P = 0.019) was lower in post-SARS-CoV-2 cases. Relative brain volume, prevalence of cerebral microbleeds, and infarct residuals were similar, while the mean cortical thickness was higher in post-SARS-CoV-2 cases. Cognitive function was not impaired. Similarly, patient-related outcomes did not differ. Conclusion Subjects who apparently recovered from mild to moderate SARS-CoV-2 infection show signs of subclinical multi-organ affection related to pulmonary, cardiac, thrombotic, and renal function without signs of structural brain damage, neurocognitive, or quality-of-life impairment. Respective screening may guide further patient management. Published in European Heart Journal (Jan. 06, 2022): https://doi.org/10.1093/eurheartj/ehab914

|
Scooped by
Juan Lama
|
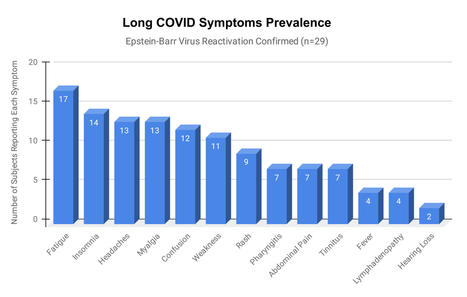
Epstein-Barr virus (EBV) reactivation resulting from the inflammatory response to coronavirus infection may be the cause of previously unexplained long COVID symptoms—such as fatigue, brain fog, and rashes—that occur in approximately 30% of patients after recovery from initial COVID-19 infection. The first evidence linking EBV reactivation to long COVID, as well as an analysis of long COVID prevalence, is outlined in a new long COVID study published in the journal Pathogens. "We ran EBV antibody tests on recovered COVID-19 patients, comparing EBV reactivation rates of those with long COVID symptoms to those without long COVID symptoms," said lead study author Jeffrey E. Gold of World Organization. "The majority of those with long COVID symptoms were positive for EBV reactivation, yet only 10% of controls indicated reactivation." The researchers began by surveying 185 randomly selected patients recovered from COVID-19 and found that 30.3% had long term symptoms consistent with long COVID after initial recovery from SARS-CoV-2 infection. This included several patients with initially asymptomatic COVID-19 cases who later went on to develop long COVID symptoms. The researchers then found, in a subset of 68 COVID-19 patients randomly selected from those surveyed, that 66.7% of long COVID subjects versus 10% of controls were positive for EBV reactivation based on positive EBV early antigen-diffuse (EA-D) IgG or EBV viral capsid antigen (VCA) IgM titers. The difference was significant (p < 0.001, Fisher's exact test). "We found similar rates of EBV reactivation in those who had long COVID symptoms for months, as in those with long COVID symptoms that began just weeks after testing positive for COVID-19," said coauthor David J. Hurley, Ph.D., a professor and molecular microbiologist at the University of Georgia. "This indicated to us that EBV reactivation likely occurs simultaneously or soon after COVID-19 infection." The relationship between SARS-CoV-2 and EBV reactivation described in this study opens up new possibilities for long COVID diagnosis and treatment. The researchers indicated that it may be prudent to test patients newly positive for COVID-19 for evidence of EBV reactivation indicated by positive EBV EA-D IgG, EBV VCA IgM, or serum EBV DNA tests. If patients show signs of EBV reactivation, they can be treated early to reduce the intensity and duration of EBV replication, which may help inhibit the development of long COVID. "As evidence mounts supporting a role for EBV reactivation in the clinical manifestation of acute COVID-19, this study further implicates EBV in the development of long COVID," said Lawrence S. Young, Ph.D., a virologist at the University of Warwick, and Editor-in-Chief of Pathogens. "If a direct role for EBV reactivation in long COVID is supported by further studies, this would provide opportunities to improve the rational diagnosis of this condition and to consider the therapeutic value of anti-herpesvirus agents such as ganciclovir." Original findings published in Pathogens (June 10, 2021): https://doi.org/10.3390/pathogens10060763

|
Scooped by
Juan Lama
|
Using cardiac MRI, researchers found myocardial injury in more than half of patients hospitalized with severe COVID-19 and elevated troponin a few months after hospital discharge. “We found evidence of high rates of heart muscle injury that could be seen on the scans a month or two after discharge. Whilst some of this may have been preexisting, MRI scanning shows that some were new, and likely caused by COVID-19,” Marianna Fontana, MD, PhD, professor of cardiology at University College London, said in a press release. “Importantly, the pattern of damage to the heart was variable, suggesting that the heart is at risk of different types of injury. While we detected only a small amount of ongoing injury, we saw injury to the heart that was present even when the heart’s pumping function was not impaired and might not have been picked up by other techniques. In the most severe cases, there are concerns that this injury may increase the risks of heart failure in the future, but more work is needed to investigate this further.” For this analysis, researchers included 148 patients from six hospitals (mean age, 64 years; 70% men) with severe COVID-19 infection and elevated troponin levels, all requiring hospitalization (32% requiring mechanical ventilation), who underwent convalescent cardiac MRI and adenosine stress perfusion at a median of 68 days after discharge. “Raised troponin levels are associated with worse outcomes in COVID-19 patients. Patients with severe COVID-19 disease often have preexisting heart-related health problems, including diabetes, raised blood pressure and obesity,” Fontana said in the release. “During severe COVID-19 infection, however, the heart may also be directly affected. Unpacking how the heart can become damaged is difficult, but MRI scans of the heart can identify different patterns of injury, which may enable us to make more accurate diagnoses and to target treatments more effectively.” Myocardial injury in COVID-19 Patients with abnormal troponin levels were offered a cardiac MRI after discharge and were compared with a control group of patients who did not have COVID-19 and 40 healthy volunteers. Researchers observed that left ventricular function was normal in 89% of the overall cohort (mean ejection fraction, 67%). Late gadolinium enhancement and/or ischemia was found in 54% of participants hospitalized for severe COVID-19 infection, which included a myocarditis-like scar in 26%, MI and/or ischemia in 22% and dual pathology in 6%. According to the study, myocarditis-like injury was limited to three or fewer myocardial segments in 88% of patients with no LV dysfunction, of which 30% had active myocarditis. In addition, MI was observed in 19% and inducible ischemia in 26% of patients who underwent stress perfusion after discharge. Moreover, of patients with ischemic injury, 66% had no prior history of coronary disease. Researchers found no evidence of diffuse fibrosis or edema in the remote myocardium. Two new opportunities “These findings give us two opportunities,” Fontana said in the release. “Firstly, to find ways of preventing the injury in the first place, and from some of the patterns we have seen, blood clotting may be playing a role, for which we have potential treatments. Secondly, detecting the consequences of injury during convalescence may identify subjects who would benefit from specific supporting drug treatments to protect heart function over time.” Findings published in European Heart Journal (Feb. 18, 2021): https://doi.org/10.1093/eurheartj/ehab075

|
Scooped by
Juan Lama
|
By early January, 2021, COVID-19, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), had resulted in more than 83 million confirmed cases and more than 1·8 million deaths. The clinical spectrum of SARS-CoV-2 infection is wide, encompassing asymptomatic infection, fever, fatigue, myalgias, mild upper respiratory tract illness, severe life-threatening viral pneumonia requiring admission to hospital, and death. Physicians are observing persisting symptoms and unexpected, substantial organ dysfunction after SARS-CoV-2 infection in an increasing number of patients who have recovered, as previously observed in the SARS outbreak. However, COVID-19 is a new disease and uncertainty remains regarding the possible long-term health sequelae. This is particularly relevant for patients with severe symptoms, including those who required mechanical ventilation during their hospital stay, for whom long-term complications and incomplete recovery after discharge would be expected. Unfortunately, few reports exist on the clinical picture of the aftermath of COVID-19. The study by Chaolin Huang and colleagues in The Lancet is relevant and timely. They describe the clinical follow-up of a cohort of 1733 adult patients (48% women, 52% men; median age 57·0 years, IQR 47·0–65·0) with COVID-19 who were discharged from Jin Yin-tan Hospital (Wuhan, China). 6 months after illness onset, 76% (1265 of 1655) of the patients reported at least one symptom that persisted, with fatigue or muscle weakness being the most frequently reported symptom (63%, 1038 of 1655). More than 50% of patients presented with residual chest imaging abnormalities. Disease severity during the acute phase was independently associated with the extent of lung diffusion impairment at follow-up (odds ratio 4·60, 95% CI 1·85–11·48), with 56% (48 of 86) of patients requiring high-flow nasal cannula, non-invasive ventilation, and invasive mechanical ventilation during their hospital stay having impaired pulmonary diffusion capacity. These findings are consistent with those from earlier small studies that reported lingering radiological and pulmonary diffusion abnormalities in a sizeable proportion of COVID-19 patients up to 3 months after hospital discharge. Evidence from previous coronavirus outbreaks suggests that some degree of lung damage could persist, as shown in patients who recovered from SARS, 38% of whom had reduced lung diffusion capacity 15 years after infection. Although SARS-CoV-2 primarily affects the lungs, several other organs, including the kidney, can also be affected. Therefore, Huang and colleagues assessed the sequelae of extrapulmonary manifestations of COVID-19. Unexpectedly, 13% (107 of 822) of the patients who did not develop acute kidney injury during their hospital stay and presented with normal renal function, based on estimated glomerular filtration rate (eGFR) during the acute phase, exhibited a decline in eGFR (<90 mL/min per 1·73 m2) at follow-up. However, this finding must be interpreted with caution... Original findings published in the Lancet (Jan. 8, 2021):

|
Scooped by
Juan Lama
|
An analysis of Ebola survivors in Sierra Leone revealed that patients with post-Ebola syndrome experience clusters of symptoms that occur together, including some with a seemingly rheumatologic pattern of disease, researchers reported.“Ebola survivors have a broad array of symptoms that fall into distinct patterns. One of these patterns resembles rheumatologic disease and may be related to gut dysfunction,” Sarah Talia Himmelfarb, MD, a resident in internal medicine and pediatrics at Tulane University School of Medicine, explained to Healio. Research has shown that Ebola survivors may face long-term health effects from the illness. “To date,” Himmelfarb said, “several studies have been performed to determine if specific markers of inflammation are associated with post-Ebola syndrome. No marker has been identified when looking at survivors as a homogeneous group.” To identify patterns within the variety of symptoms experienced by Ebola survivors, Himmelfarb and colleagues identified survivors in Eastern Sierra Leone through the Sierra Leone Association of Ebola Survivors and household contacts of survivors and recruited them for a study. Himmelfarb presented findings from the study at IDWeek. Participants from both groups received a questionnaire regarding self-reported symptoms and underwent a physical exam. The researchers compared symptoms between the groups and analyzed correlations between clusters. “Our motivation in doing this was to see if any patterns fit known disease processes,” Himmelfarb said. “In particular, we wanted to investigate the possibility that they fit the pattern of a rheumatologic or autoimmune disease. This would help us better understand this poorly characterized syndrome and might help lead to therapies for those who suffer from it.” Between March 2016 and January 2019, 375 Ebola survivors and 1,040 contacts were enrolled in the study. According to Himmelfarb and colleagues, at the time of enrollment, Ebola survivors across all age groups reported significantly more symptoms than contacts in all categories. The researchers identified six symptom clusters “representing distinct organ systems” and two general phenotypes with or without rheumatologic symptoms. According to the study, clusters including rheumatologic symptoms were correlated with one another (r = 0.63) but not with other clusters (r < 0.35). Additionally, ophthalmologic/auditory symptoms were moderately correlated with the nonrheumatologic clusters (r > 0.5), whereas psychologic/neurologic, cardiac/gastrointestinal and constitutional clusters correlated with one another (r >0.6) in all cases. After mapping the symptom clusters, the researchers determined that each symptom cluster was separated from the rest, particularly the phenotypes with rheumatologic symptoms. The group of survivors with the seemingly rheumatologic pattern of disease complained of symptoms that included joint pain and decreased range of motion, Himmelfarb said. This group overlapped with a group with gastroenterological symptoms, such as abdominal tenderness. “An intriguing possibility is that inflammation stemming from impaired gut barrier, as was detected in a previous study, may be an etiologic cause of this group of symptoms,” Himmelfarb said. “This work has significance for the thousands of Ebola survivors who emerged from the 2014-2016 epidemic in Western Africa. It also contributes a small but growing body of knowledge of post-viral sequelae. This field has only become more relevant in the age of COVID-19.”
|

|
Scooped by
Juan Lama
|
Background Long COVID is a post-severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection syndrome characterised by not recovering for several weeks or months following the acute episode. The effectiveness of COVID-19 vaccines against long-term symptoms of COVID-19 is not well understood. We determined whether vaccination was associated with the incidence of reporting long-term symptoms post-SARS-CoV-2 infection Methods We invited individuals who were PCR tested for SARS-CoV-2 infection at participating hospitals between March 2020-November 2021 to fill an online questionnaire that included baseline demographics, details of their acute episode and information about symptoms they were currently experiencing. Using binomial regression, we compared vaccinated individuals with those unvaccinated and those uninfected in terms of self-reported symptoms post-acute infection. Results We included 951 infected and 2437 uninfected individuals. Of the infected, 637(67%) were vaccinated. The most commonly reported symptoms were; fatigue (22%), headache (20%), weakness (13%), and persistent muscle pain (10%). After adjusting for follow-up time and baseline symptoms, those who received two doses less likely than unvaccinated individuals to report any of these symptoms by 64%, 54%, 57%, and 68% respectively, (Risk ratios 0.36, 0.46, 0.43, 0.32, p<0.04 in the listed sequence). Those who received two doses were no more likely to report any of these symptoms than individuals reporting no previous SARS-CoV-2 infection. Conclusions Vaccination with at least two doses of COVID-19 vaccine was associated with a substantial decrease in reporting the most common post-acute COVID-19 symptoms, bringing it back to baseline. Our results suggest that, in addition to reducing the risk of acute illness, COVID-19 vaccination may have a protective effect against long COVID. Preprint available in medRxiv (Jan. 17, 2022): https://doi.org/10.1101/2022.01.05.22268800

|
Scooped by
Juan Lama
|
One year after becoming ill with the coronavirus, nearly half of patients in a large new study were still experiencing at least one lingering health symptom, adding to evidence that recovery from COVID-19 can be arduous and that the multifaceted condition known as “long COVID” can last for months. The study, published Thursday in the journal Lancet, is believed to be the largest to date in which patients were evaluated one year after being hospitalized for COVID. It involved 1,276 patients admitted to Jin Yin-tan Hospital in Wuhan, China, who were discharged between Jan. 7 and May 29, 2020. The researchers, who also evaluated the patients six months after hospitalization, found that while many symptoms improved over time and many of the 479 people who had been employed when they got COVID had returned to their original job, 49% of patients still had at least one health problem. And shortness of breath and mental health issues such as anxiety or depression were slightly more prevalent 12 months later than at the six-month mark, the researchers reported, saying the reasons for that “worrying” increase were unclear. The researchers also compared the patients in the study with people in the community who had not had COVID but had similar preexisting health conditions and other characteristics. After 12 months, COVID survivors had worse overall health than people who had not been infected. They were also much more likely to be experiencing pain or discomfort, anxiety or depression, and mobility problems than those who had not had the disease. The patients, whose median age was 57, were given physical exams, lab tests and a standard measure of endurance and aerobic capacity called a 6-minute walk test. They were also interviewed about their health. The study involved patients who were sick enough to be hospitalized, but who were generally not the most severely debilitated. About 75% required supplemental oxygen when they were hospitalized, but most did not need intensive care, ventilators or even high-flow nasal oxygen, a noninvasive method. Women were more likely than men to have some lingering symptoms, including mental health issues and lung function problems. One of the most common symptoms was fatigue or muscle weakness, reported by 20% of patients. But that represented a significant decrease from the 52% who reported such symptoms six months after hospitalization. Some issues, such as shortness of breath, were more common in people who had been more severely ill. But some issues did not correlate to severity of the initial illness. For example, 244 patients underwent a lung-function test, which found that from six months to one year after hospitalization, there was no decrease in the proportion of patients with reduced flow of oxygen from their lungs to their bloodstream — regardless of how ill the patients had been initially. “The need to understand and respond to long COVID is increasingly pressing,” said an editorial that Lancet published about the study. “Symptoms such as persistent fatigue, breathlessness, brain fog and depression could debilitate many millions of people globally.” It added: “Long COVID is a modern medical challenge of the first order.” Study Cited Published in The Lancet (Aug. 28, 2021): https://doi.org/10.1016/S0140-6736(21)01755-4

|
Scooped by
Juan Lama
|
An analysis of electronic medical records in California found that 32 percent started with asymptomatic infections but reported troubling aftereffects weeks and months later. The study, one of the first to focus exclusively on people who never needed to be hospitalized when they were infected, analyzed electronic medical records of 1,407 people in California who tested positive for the coronavirus. More than 60 days after their infection, 27 percent, or 382 people, were struggling with post-Covid symptoms like shortness of breath, chest pain, cough or abdominal pain. Nearly a third of the patients with such long-term problems had not had any symptoms from their initial coronavirus infection through the 10 days after they tested positive, the researchers found. Understanding long-term Covid symptoms is an increasingly pressing priority for doctors and researchers as more and more people report debilitating or painful aftereffects that hamper their ability to work or function the way they did before. Last month, the director of the National Institutes of Health, Dr. Francis S. Collins, announced a major initiative “to identify the causes and ultimately the means of prevention and treatment of individuals who have been sickened by Covid-19, but don’t recover fully over a period of a few weeks.” David Putrino, director of rehabilitation innovation at Mount Sinai Health System in New York City, who was not involved in the new research, said that he and his colleagues at Mount Sinai’s center for post-Covid care are seeing a similar pattern. “Many people who had asymptomatic Covid can also go on to develop post-acute Covid syndrome,” said Dr. Putrino, who is a co-author of a smaller study on the topic published last year. “It doesn’t always match up with severity of acute symptoms, so you can have no symptoms but still have a very aggressive immune response.” The new study is published on the preprint site MedRxiv and has not finished undergoing peer review. Its strengths include that it is larger than many studies on long-term symptoms published so far and that the researchers used electronic records from the University of California system, allowing them to obtain health and demographic information of patients from throughout the state. The researchers also excluded from the study symptoms that patients had reported in the year before their infection, a step intended to ensure a focus on post-Covid symptoms. Among their findings: Long-term problems affect every age group, including children. “Of the 34 children in the study, 11 were long-haulers,” said one of the authors, Melissa Pinto, an associate professor of nursing at the University of California Irvine. The study found more than 30 symptoms, including anxiety, low back pain, fatigue, insomnia, gastrointestinal problems and rapid heart rate. The researchers identified five clusters of symptoms that seemed most likely to occur together, like chest pain and cough or abdominal pain and headache. Most previous studies of long-term symptoms have tended to involve people who were sick enough from their initial infection to be hospitalized. One of the largest found that more than three-quarters of about 1,700 hospitalized patients in Wuhan, China, had at least one symptom six months later. But increasingly, people who were never hospitalized are seeking care at post-Covid clinics, and scientists are recognizing the need to understand their circumstances. Last month, researchers at the University of Washington reported on a survey of 177 people who had tested positive for the coronavirus. Most of them had not been hospitalized. About a third of both the people who had been hospitalized and the people who had only mild initial illnesses reported having at least one lasting symptom six months later, the researchers found. Unlike some recent surveys, like one by a patient-led research team, the new study did not capture one of the most commonly reported “long Covid” issues: cognitive problems like brain fog, memory problems and difficult concentrating. One of the co-authors, Natalie Lambert, an associate research professor at Indiana University School of Medicine, said that may be because at the time, doctors may not have known to include diagnostic codes for such cognitive issues in the medical records of Covid patients. The team is seeking funding for a larger and more comprehensive study that combines information in medical records, doctors’ notes and patients’ reports, she said. In the new study, about 59 percent of the patients with long-term symptoms were women, and about half of the patients were Hispanic and 31 percent were white. The authors and Dr. Putrino cautioned that any reliable demographic conclusions would require bigger studies that are national in scope. Dr. Lambert said it was likely that the medical records used in the study reflected only a percentage of people who had asymptomatic Covid infections and experienced Covid aftereffects. “For some people, if they’re asymptomatic and they don’t know that they’re sick, they’re not going to go get tested,” she said. “Another important component is that we know that some of the long-haul symptoms show up much later than two months,” Dr. Lambert said. “So there’s a potential for a wide range of long-haul symptoms that they’re not going to associate with Covid.” Dr. Pinto said it would be important to study the condition over time, instead of in a static snapshot. “The long haul is a very dynamic process and symptoms can change from day to day,” she said. “One day they may have chest pain and a headache, and the very next day, the chest pain and headache is gone and they have backache and muscle aches. We need to capture trajectory and changing of symptoms across time, and we need this in a larger sample that represents America.” Cited study poosted in medRxiv (March 5, 2021): https://doi.org/10.1101/2021.03.03.21252086

|
Scooped by
Juan Lama
|
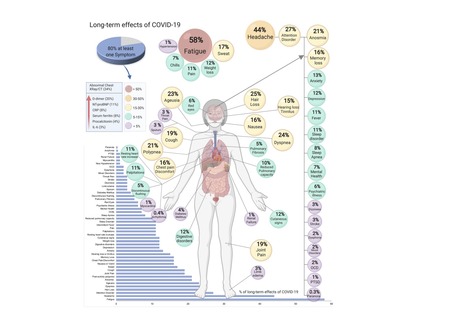
COVID-19, caused by SARS-CoV-2, can involve sequelae and other medical complications that last weeks to months after initial recovery, which has come to be called Long-COVID or COVID long-haulers. This systematic review and meta-analysis aims to identify studies assessing long-term effects of COVID-19 and estimates the prevalence of each symptom, sign, or laboratory parameter of patients at a post-COVID-19 stage. LitCOVID (PubMed and Medline) and Embase were searched by two independent researchers. All articles with original data for detecting long-term COVID-19 published before 1st of January 2021 and with a minimum of 100 patients were included. For effects reported in two or more studies, meta-analyses using a random-effects model were performed using the MetaXL software to estimate the pooled prevalence with 95% CI. Heterogeneity was assessed using I2 statistics. The Preferred Reporting Items for Systematic Reviewers and Meta-analysis (PRISMA) reporting guideline was followed. A total of 18,251 publications were identified, of which 15 met the inclusion criteria. The prevalence of 55 long-term effects was estimated, 21 meta-analyses were performed, and 47,910 patients were included. The follow-up time ranged from 15 to 110 days post-viral infection. The age of the study participants ranged between 17 and 87 years. It was estimated that 80% (95% CI 65-92) of the patients that were infected with SARS-CoV-2 developed one or more long-term symptoms. The five most common symptoms were fatigue (58%), headache (44%), attention disorder (27%), hair loss (25%), and dyspnea (24%). All meta-analyses showed medium (n=2) to high heterogeneity (n=13). In order to have a better understanding, future studies need to stratify by sex, age, previous comorbidities, severity of COVID-19 (ranging from asymptomatic to severe), and duration of each symptom. From the clinical perspective, multi-disciplinary teams are crucial to developing preventive measures, rehabilitation techniques, and clinical management strategies with whole-patient perspectives designed to address long COVID-19 care. Preprint available in medRxiv (Jan. 30, 2021): https://doi.org/10.1101/2021.01.27.21250617

|
Scooped by
Juan Lama
|
A new study in the American Journal of Preventive Medicine presents new data that address important questions pertaining to the containment of the coronavirus pandemic: When should COVID-19 quarantine really end and which continuing symptoms may be more indicative of a positive test in recovered patients? The study was conducted by the Fondazione Policlinico Universitario "Agostino Gemelli" IRCCS, Rome, Italy, where a multidisciplinary healthcare service was established for all patients who have recovered from COVID-19 to study what happens to them after recovery and to assess the impact of the virus on their bodies. Investigators report that close to 17 percent of patients considered fully recovered from COVID-19 tested positive for the virus in follow-up screening. Patients who continued to have respiratory symptoms, especially sore throat and rhinitis, were more likely to have a new positive test result. This suggests the persistence of these two symptoms should not be underestimated and should be adequately assessed in all patients considered recovered from COVID-19. "Clinicians and researchers have focused on the acute phase of COVID-19, but continued monitoring after discharge for long-lasting effects is needed," explained lead investigator Francesco Landi, MD, Ph.D., Fondazione Policlinico Universitario "Agostino Gemelli" IRCCS, and Catholic University of the Sacred Heart, Rome, Italy. The study included 131 patients who met the World Health Organization (WHO) criteria for discontinuation of quarantine at least two weeks prior to the follow-up visit. The WHO criteria specify that the patient should be fever-free without fever-reducing medications for three days, show improvement in any symptoms related to COVID-19, be more than seven days past symptom onset, and test negative for the SARS-CoV-2 virus twice, at least 24 hours apart, with reverse transcription PCR (RT-PCR) testing. A new RT-PCR test was administered at the time of post-acute care admission. Demographic, medical, and clinical information was collected, with an emphasis on the persistence of symptoms and signs related to COVID-19 such as cough, fatigue, diarrhea, headache, smelling disorders, loss of appetite, sore throat, and rhinitis. Twenty-two (16.7 percent) of the patients tested positive again. There was no significant difference between patients with positive and negative test results in terms of age or sex. None of the patients had fever and all reported improvement in their overall clinical condition. Time since onset of disease, number of days hospitalized, and treatments received while hospitalized were not significant. However, some symptoms such as fatigue (51 percent), labored breathing (44 percent) and coughing (17 percent) were still present in a significant percentage of the patients studied, although there were no significant differences between individuals with a positive or negative test. The only two symptoms that were higher and significantly prevalent in patients with a positive test were sore throat (18 percent vs. 4 percent) and signs of rhinitis (27 percent vs. 2 percent). Our findings indicate that a noteworthy rate of recovered patients with COVID-19 could still be asymptomatic carriers of the virus," Dr. Landi observed. "The main question for the containment of SARS-CoV-2 pandemic infection that still needs to be answered is whether persistent presence of virus fragments means the patients is still contagious. The RT-PCR test looks for small fragments of viral RNA. A positive swab test can reveal if patients are still shedding viral fragments, but it is not able to discern whether they are or aren't infectious." Importantly, the investigators recommend that for patients who continue to have symptoms potentially related to COVID-19, it is reasonable to be cautious and avoid close contact with others, wear a face mask, and possibly undergo an additional nasopharyngeal swab. Original study in JAMA (Sept. 18, 2020): https://doi.org/10.1016/j.amepre.2020.08.014

|
Scooped by
Juan Lama
|
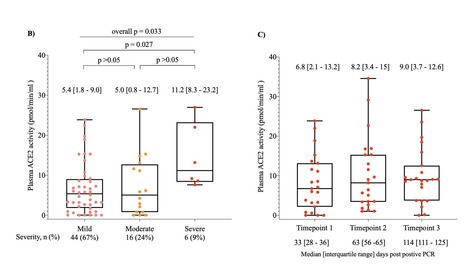
COVID-19 causes persistent endothelial inflammation, lung and cardiovascular complications. SARS-CoV-2 utilises the catalytic site of full-length membrane-bound angiotensin converting enzyme 2 (ACE2) for cell entry causing downregulation of tissue ACE2. We reported downregulation of cardiac ACE2 is associated with increased plasma ACE2 activity. In this prospective observational study in recovered COVID-19 patients, we hypothesised that SARS-CoV-2 infection would be associated with shedding of ACE2 from cell membranes and increased plasma ACE2 activity. We measured plasma ACE2 catalytic activity using a validated, sensitive quenched fluorescent substrate-based assay in a cohort of Australians aged 18 years and over who had recovered from mild, moderate or severe SARS-CoV-2 infection (positive result by PCR testing) (n=66) and age and gender matched uninfected controls (n=70). Serial samples were available in 23 recovered SARS-CoV-2 patients. Plasma ACE2 activity at a median of 35 days post-infection [interquartile range 30-38 days] was 97-fold higher in recovered SARS-CoV-2 patients compared to controls (5.8 [2-11.3] vs. 0.06 [0.02-2.2] pmol/min/ml, p<0.0001). There was a significant difference in plasma ACE2 activity according to disease severity (p=0.033), with severe COVID-19 associated with higher ACE2 activity compared to mild disease (p=0.027). Men (n=39) who were SARS-CoV-2 positive had higher median plasma ACE2 levels compared to women (n=27) (p<0.0001). We next analysed whether an elevated plasma ACE2 activity level persisted following SARS-CoV-2 infection in subjects with blood samples at 63 [56-65] and 114 [111-125] days post infection. Plasma ACE2 activity remained persistently elevated in almost all subjects, with no significant differences between timepoints in post-hoc comparisons (p>0.05). This is the first description that plasma ACE2 activity is elevated after COVID-19 infection, and the first with longitudinal data indicating plasma ACE2 activity remains elevated out to a median of 114 days post- infection. Larger studies are now needed to determine if persistent elevated plasma ACE2 activity identifies people at risk of prolonged illness following COVID-19. Preprint available at medRxiv (October 8, 2020): https://doi.org/10.1101/2020.10.06.20207514
|



 Your new post is loading...
Your new post is loading...