Saliva Specimens to Detect SARS-CoV-2 Infection In this letter, the investigators report that saliva specimens and nasopharyngeal swab specimens had similar sensitivity in the detection of COVID-19. Rapid and accurate diagnostic tests are essential for controlling the ongoing Covid-19 pandemic. Although the current standard involves testing of nasopharyngeal swab specimens by quantitative reverse-transcriptase polymerase chain reaction (RT-qPCR) to detect SARS-CoV-2, saliva specimens may be an alternative diagnostic sample. Rigorous evaluation is needed to determine how saliva specimens compare with nasopharyngeal swab specimens with respect to sensitivity in detection of SARS-CoV-2 during the course of infection.
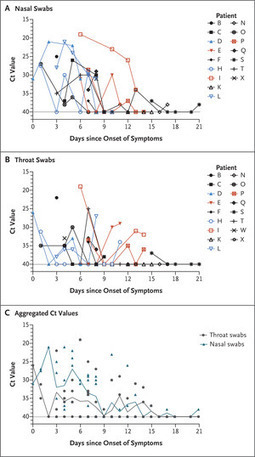
A total of 70 inpatients with Covid-19 provided written informed consent to participate in our study available with the full text of this letter at NEJM.org). After Covid-19 was confirmed with a positive nasopharyngeal swab specimen at hospital admission, we obtained additional samples from the patients during hospitalization. We tested saliva specimens collected by the patients themselves and nasopharyngeal swabs collected from the patients at the same time point by health care workers. Using primer sequences from the Centers for Disease Control and Prevention, we detected more SARS-CoV-2 RNA copies in the saliva specimens (mean log copies per milliliter, 5.58; 95% confidence interval [CI], 5.09 to 6.07) than in the nasopharyngeal swab specimens (mean log copies per milliliter, 4.93; 95% CI, 4.53 to 5.33). In addition, a higher percentage of saliva samples than nasopharyngeal swab samples were positive up to 10 days after the Covid-19 diagnosis. At 1 to 5 days after diagnosis, 81% (95% CI, 71 to 96) of the saliva samples were positive, as compared with 71% (95% CI, 67 to 94) of the nasopharyngeal swab specimens. These findings suggest that saliva specimens and nasopharyngeal swab specimens have at least similar sensitivity in the detection of SARS-CoV-2 during the course of hospitalization...
Published in New England J. Medicine (August 28, 2020):



 Your new post is loading...
Your new post is loading...