For hundreds of thousands of years, monkeys and apes have been plagued by simian immunodeficiency virus (SIV), which still devastates primate groups in Africa. Luckily, as humans evolved from these early primates, we picked up a mutation that made us immune from SIV — at least until the early 20th century, when the virus evolved to get around our defenses, giving rise to human immunodeficiency virus (HIV) and an AIDS pandemic that today affects an estimated 38 million people worldwide. University of California, Berkeley, researchers have now discovered how that long-ago human mutation interfered with SIV infection, a finding that could provide clues for the development of new therapies to thwart HIV and similar viral infections.
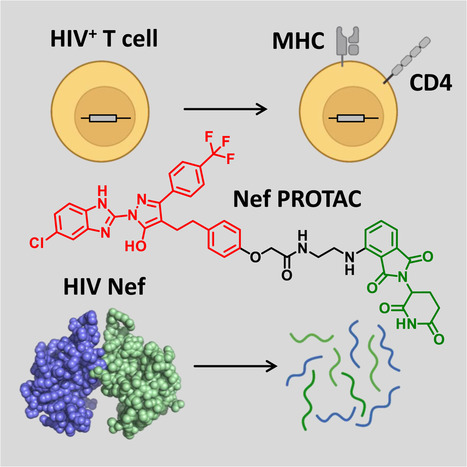
The barrier was a mutation in human cells that blocked SIV from forcing these cells to shed thousands more copies of the virus. As a result, humans could not re-infect one another. This genetic mutation interfered with the ability of an SIV protein to tightly bind two human proteins and send them for destruction within the cell, instead of fighting the virus. The researchers used cryo-electron microscopy, or cryoEM, to determine the structure of this protein complex and discovered that the mutation so effectively disrupted the protein binding sites that it took SIV a long time to find a work-around.
“The binding site involved is structurally very complex, so essentially it is not possible to adapt to it once the tight binding is lost. The virus had to invent a completely different way to do the same thing, which took a long time in evolution,” Hurley said. “This conferred an advantage on our prehistoric ancestors: From chimps on down, every primate was susceptible to SIV, but humans were immune. That gave humans probably a grace period of tens to hundreds of thousands of years to develop without having to deal with this disease. I tend to think that really gave a leg up to humans in early evolution.”
Because budding is an important step in the spread of many viruses, primates long ago evolved natural defenses, including proteins on the surface of cells that staple the budding virions to the cell and prevent them from leaving. As they accumulate, the immune system recognizes these unbudded virions as abnormal and destroys the whole cell, virus and all. In monkey, ape and human cells, the staple is called tetherin, because it tethers the budding virion to the cell membrane. In the constant arms race between host and pathogen, SIV evolved a countermeasure that exploits another normal cell function: its recycling system. Cells have ways to remove proteins sitting on the surface, through which cells constantly take up and recycle tetherin if there’s no indication it is needed to fight an invading virus. It does this by dimpling the membrane inward to form a little bubble inside the cell, capturing tetherin and other surface proteins in this vesicle and then digesting all the contents, including tetherin. SIV’s countermeasure was to produce a protein, called Nef, that revs up the recycling of tetherin, even during an infection. This enables virions to bud off and search for new victims.
Results published online August 22, 2019 in Cell Host & Microbe:
https://doi.org/10.1016/j.chom.2019.08.002



 Your new post is loading...
Your new post is loading...