Your new post is loading...

|
Scooped by
Juan Lama
|
The alert comes after a man diagnosed with Crimean-Congo haemorrhagic fever (CCHF) was hospitalised, pushing the health officials to generate an alert. British tourists and expats in Spain have been issued an urgent warning about a deadly virus that kills 40 percent of the infected ones The alert comes after a man diagnosed with Crimean-Congo haemorrhagic fever (CCHF) was hospitalised, pushing the health officials to generate an alert. The Spanish Castile and León Ministry of Health confirmed that the patient is in a critical but stable condition. The disease, typically transmitted by ticks, is clinically associated with several symptoms, health bodies have revealed. Medical experts at Travel Health Pro told GB news: “The patient remains admitted, stable in serious conditions, at the Salamanca Hospital, where the protocolized epidemiological and care measures have been adopted.” The confirmed case is an elderly man, who has been admitted to hospital in Salamanca Hospital, in Northwestern Spain. “He has a tick bite and remains stable, although with the clinical severity that this pathology implies, with the isolation measures and protection of health professionals provided for these situations,” added Travel Health Pro. According to the WHO, the CCHF virus is transmitted to people either by tick bites or through contact with an infected animal's blood. The health body adds: “The majority of cases have occurred in people involved in the livestock industry, such as agricultural workers, slaughterhouse workers and veterinarians.” Anyone who has experienced symptoms or believes they may have been exposed to CCHF has been told to seek advice from a GP or NHS 111. “Remember - tell your healthcare providers that you travelled abroad,” said Travel Health Pro. In patients who recover from the disease, improvements tend to start around the ninth day or tenth day after the onset of illness. The WHO said: “It is difficult to prevent or control CCHF infection in animals and ticks as the tick-animal-tick cycle usually goes unnoticed and the infection in domestic animals is usually not apparent. “Furthermore, the tick vectors are numerous and widespread, so tick control with acaricides (chemicals intended to kill ticks) is only a realistic option for well-managed livestock production facilities. “There are no vaccines widely available for human or animal use. In the absence of a vaccine, the only way to reduce infection in people is by raising awareness of the risk factors and educating people about the measures they can take to reduce exposure to the virus.”

|
Scooped by
Juan Lama
|
Background At least 5–10% of subjects surviving COVID-19 develop the post-COVID-19 condition (PCC) or “Long COVID”. The clinical presentation of PCC is heterogeneous, its pathogenesis is being deciphered, and objective, validated biomarkers are lacking. It is unknown if PCC is a single entity or a heterogeneous syndrome with overlapping pathophysiological basis. The large US RECOVER study identified four clusters of subjects with PCC according to their presenting symptoms. However, the long-term clinical implications of PCC remain unknown. Methods We conducted a 2-year prospective cohort study of subjects surviving COVID-19, including individuals fulfilling the WHO PCC definition and subjects with full clinical recovery. We systematically collected post-COVID-19 symptoms using prespecified questionnaires and performed additional diagnostic imaging tests when needed. Factors associated with PCC were identified and modelled using logistic regression. Unsupervised clustering analysis was used to group subjects with PCC according to their presenting symptoms. Factors associated with PCC recovery were modelled using a direct acyclic graph approach. Findings The study included 548 individuals, 341 with PCC, followed for a median of 23 months (IQR 16.5–23.5), and 207 subjects fully recovered. In the model with the best fit, subjects who were male and had tertiary studies were less likely to develop PCC, whereas a history of headache, or presence of tachycardia, fatigue, neurocognitive and neurosensitive complaints and dyspnea at COVID-19 diagnosis predicted the development of PCC. The cluster analysis revealed the presence of three symptom clusters with an additive number of symptoms. Only 26 subjects (7.6%) recovered from PCC during follow-up; almost all of them (n = 24) belonged to the less symptomatic cluster A, dominated mainly by fatigue. Recovery from PCC was more likely in subjects who were male, required ICU admission, or had cardiovascular comorbidities, hyporexia and/or smell/taste alterations during acute COVID-19. Subjects presenting with muscle pain, impaired attention, dyspnea, or tachycardia, conversely, were less likely to recover from PCC. Interpretation Preexisting medical and socioeconomic factors, as well as acute COVID-19 symptoms, are associated with the development of and recovery from the PCC. Recovery is extremely rare during the first 2 years, posing a major challenge to healthcare systems. Published in The Lancet Regional Health (Sept. 4, 2023):

|
Scooped by
Juan Lama
|
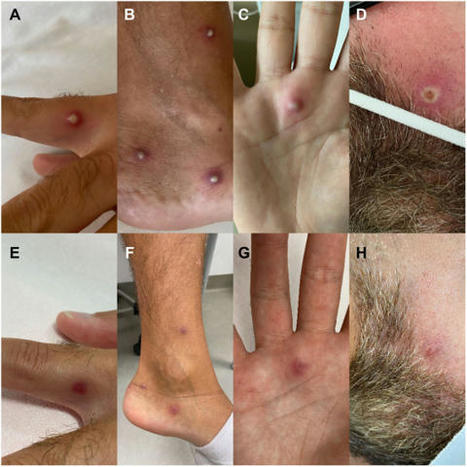
In this journal E. Orviz and colleagues recently described the clinical presentation of the first monkeypox patients in Spain, highlighting the frequent co-presence of sexually transmitted infections (STI). To date, no reports of co-infection with monkeypox virus and SARS-CoV-2 have been published. Therefore, in this study we present the clinical features and diagnostic procedure of the first documented case of co-infection with monkeypox virus, SARS-CoV-2 and HIV-1. Since January 2022, more than 16,000 people in over 74 countries have been affected by monkeypox, prompting the World Health Organization to declare this outbreak a public health emergency of international concern. Human-to-human transmission occurs through close contact with infectious material from skin lesions, fomites, seminal fluids and oropharyngeal secretions. The majority of cases were registered in gay or bisexual men often suffering from other STI. At the same time, SARS-CoV-2 is still a major cause of morbidity and mortality globally. COVID-19 shares with monkeypox both the transmission by air droplets and the symptoms of fever, lymphadenopathy, headache, sore throat and fatigue. As these pathogens continue to spread, individuals can be simultaneously infected with monkeypox virus, SARS-CoV-2 and STI, making it difficult for physicians to perform the correct diagnosis, also considering that not all patients with monkeypox develop skin lesions. Our patient, an Italian 36-year-old male spent 5 days in Spain from 16 to 20 June 2022 (Figure 1). Nine days after, he developed fever (up to 39°C), accompanied by sore throat, fatigue, headache and right inguinal lymphadenomegaly. On 2 July he resulted positive for SARS-CoV-2. On the afternoon of the same day a rash started to develop on his left arm. The following day small, painful vesicles surrounded by an erythematous halo appeared on the torso, lower limbs, face and glutes. On 5 July, due to a progressive and uninterrupted spread of vesicles that began to evolve into umbilicated pustules, he went to the emergency department of the Policlinico “G. Rodolico - San Marco” University Hospital in Catania, Italy, and was subsequently transferred to the Infectious Diseases unit. On admission, the patient reported being treated for syphilis in 2019. In September 2021, he performed an HIV test with a negative result. He suffered from bipolar disorder, for which he regularly took carbamazepine 200 mg daily. He was vaccinated for SARS-CoV-2 with two doses of Pfizer's BNT162b2 mRNA vaccine (the last in December 2021) and had already contracted COVID-19 in January 2022. He also reported of having condomless intercourse with men during his stay in Spain. Fever (37.5°C), pharyngodynia, fatigue, headache was still present. On physical examination his body was dotted, including the palm of the right hand and the perianal region, with skin lesions in various stages of progression, ranging from small vesicles (Figure 1, Panel A) to reddened haloed pustules (Figure 1, Panel B and Panel C) and umbilicated plaques (Figure 1, Panel D). The oral mucosa was normal, except for bilateral tonsillar hypertrophy. A modest hepatosplenomegaly and an enlarged (2 cm), hypomobile and painful lymph node in the right inguinal region were found. Laboratory test showed elevated C-reactive protein (69 mg/L, normal values 0.0 - 5.0 mg/L), fibrinogen (713 mg/dL, normal values 170 - 400 mg/dL) and prothrombin time (1.21, normal values 0.8 - 1.2). Chest X-ray revealed a parenchymal hypodiaphany in the right parailary region... Published in Journal of Infection (August 19, 2022):

|
Scooped by
Juan Lama
|
Researchers suspect an adenovirus may be involved, but are still searching for the cause of illness. Puzzled scientists are searching for the cause of a strange and alarming outbreak of severe hepatitis in young children, with 74 cases documented in the United Kingdom and three in Spain. Clinicians in Denmark and the Netherlands are also reporting similar cases. And in the United States, the Centers for Disease Control and Prevention (CDC) said late yesterday it is investigating nine cases in Alabama. Viruses can cause hepatitis, an inflammation of the liver, but otherwise-healthy children rarely become seriously ill. As of 12 April, none of the U.K. or Spanish children have died, but some are very sick: All have been admitted to hospitals and seven required liver transplants, six of them in the United Kingdom, according to a World Health Organization (WHO) statement issued today. Two of the nine affected children in Alabama have required liver transplants, the state’s Department of Public Health announced this afternoon. The leading theory is that an adenovirus, a family of viruses that more typically cause colds, is the culprit—up to half of the sickened children in the United Kingdom tested positive for such a virus, as did all the children in Alabama. But so far, the evidence is too thin to resolve the mystery, researchers and physicians say. “This is a severe phenomenon,” says Deirdre Kelly, a pediatric hepatologist at Birmingham Children’s Hospital in the United Kingdom. “These [were] perfectly healthy children … up to a week ago.” Not all the news is bad, however. “Most of [the children] recover on their own,” Kelly notes. “This should be taken seriously,” WHO’s Regional Office for Europe wrote in an emailed statement. “The increase is unexpected and the usual causes have been excluded.” Scottish investigators first identified the outbreak on 31 March, when they alerted Public Health Scotland to a cluster of 3- to 5-year-olds admitted to the Royal Hospital for Children in Glasgow in the first 3 weeks of March. Each was diagnosed with severe hepatitis of unknown cause. Typically, Scotland sees fewer than four such cases annually, the investigators wrote in a paper published yesterday. But there have been 13 cases in Scottish children as of 12 April, all but one in March and April. Kelly, who works at one of England’s three centers for pediatric liver disease and transplantation, says that since the start of this year, her unit has seen 40 cases of childhood hepatitis of uncertain cause. Over the same January to April period in 2018, her unit saw only seven such children. Most of the U.K. children are 2 to 5 years old, according to a statement issued on 8 April by the UK Health Security Agency. The European Centre for Disease Prevention and Control issued a public alert on 12 April about the U.K. outbreak, noting that vomiting and jaundice—yellowing of the skin and the whites of the eyes—are common symptoms. Early hypotheses about what might be making the children sick included a toxic exposure from food, drinks, or toys, but suspicion now centers on a virus. None of the U.K. or Spanish kids had the hepatitis A, B, C, or E viruses, typical infectious causes of the disease. But a handful of children tested positive for SARS-CoV-2 infection shortly before or upon hospital admission; none had received a COVID-19 vaccine. In addition, as many as half had adenovirus, a common virus passed by respiratory droplets and from touching infected people or virus on surfaces. It can cause vomiting, diarrhea, conjunctivitis, and cold symptoms but rarely causes hepatitis. “The leading hypotheses center around adenovirus—either a new variant with a distinct clinical syndrome or a routinely circulating variant that is more severely impacting younger children who are immunologically naïve,” the Scottish investigators wrote. Isolation of the youngest children during the pandemic lockdown may have left them immunologically vulnerable because they haven’t been exposed to the multiplicity of viruses, including adenoviruses, that typically attend toddlerhood. “We are seeing a surge in typical childhood viral infections as children come out of lockdown, [as well as] a surge in adenovirus infections”—but can’t be sure that one is causing the other, says Will Irving, a clinical virologist at the University of Nottingham. Researchers continue to study other possibilities. For example, the immunological effects of a prior episode of COVID-19 might have left children more vulnerable to infection or the illness could be a long-term complication of COVID-19 itself. An unidentified toxin has also not been ruled out. All the cases might not have a single cause, cautions Jim McMenamin, an epidemiologist who heads the infection service of Public Health Scotland. “It’s awfully important that we ensure we are looking for everything, that we are not confining ourselves to saying this is simply one viral cause.” In the United States, CDC is helping the Alabama Department of Public Health investigate nine cases of hepatitis in children ranging in age from 1 to 6 years old and who also tested positive for adenovirus. The cases have occurred since October 2021, Kristen Nordlund, a CDC spokesperson, wrote in the statement emailed to ScienceInsider last night. “CDC is working with state health departments to see if there are additional U.S. cases, and what may be causing these cases,” she wrote. “Adenovirus may be the cause for these, but investigators are still learning more—including ruling out the more common causes of hepatitis.” Wes Stubblefield, a district medical officer with the Alabama Department of Public Health, said in an interview today that the most recent case in Alabama occurred in February, and that five of the nine children tested positive for adenovirus-41, a strain that commonly causes gastroenteritis. Meanwhile, in Spain, the government of the Madrid region announced on 13 April that three regions—Madrid, Aragón, and Castilla-La Mancha—had each reported a case of severe hepatitis of unknown origin in young children. One child has received a liver transplant. Physicians at major pediatric liver centers in the Netherlands and Denmark told ScienceInsider yesterday they are seeing similar trends. “There are children that are very sick and have been referred for transplantation,” says Ruben de Kleine, a pediatric liver transplant surgeon at University Medical Center Groningen. “We have assessed a similar number of kids for transplantation within the first 4 months of 2022 [to what we] normally do in a whole year.” At Copenhagen University Hospital, too, “we have more cases with [acute liver failure] than we normally have,” says pediatric hepatologist Marianne Hørby Jørgensen. No children there have needed transplants. Hørby Jørgensen and de Kleine both stress that parents should not panic. To date, clinicians have identified small numbers of cases in their countries where, combined, more than 230,000 infants are born each year.

|
Scooped by
Juan Lama
|
Researchers hope as well as preventing disease the immunisation will, crucially, stop transmission of the virus. Spanish scientists are preparing to start clinical trials of a Covid-19 vaccine nasal spray that they say could stop the spread of the virus as well as prevent people from falling ill. The vaccines that are currently available or close to approval, including the leading Pfizer/BioNTech jab, are all administered via injection, and while they are effective at preventing disease in someone who is infected with the virus, it is not yet clear if they stop people transmitting it. The Spanish team is one of a handful across the world working on nasal sprays as a means of delivering a vaccine. The theory is that inhalable vaccines activate the local immune response in the nose, mouth and throat and therefore stem infection here, making it less likely for people to pass the virus on. The vaccine would also deliver the wider systemic immunity that is delivered by any other candidate, the scientists say. A team in China submitted approval for trials of a similar nasal spray vaccine in the autumn, and the team from Spain's CSIC national research council plan to begin human trials early next year. Dr Luis Enjuanes, a virologist at the CSIC who has been studying coronaviruses for the past 40 years, told the Telegraph: "Where do we need the protection most? The virus is largely transmitted by us breathing in aerosols." Other leading experts said nasal sprays were a promising option. "If you stick a needle into an arm and go straight into tissue you activate a whole different set of cells than if you inhale a vaccine through the nose,” said Deborah Dunn-Walters, professor of immunology at the University of Surrey and a spokesperson for the British Society for Immunology. "With a respiratory virus you have the nose, mouth and lungs which have mucosal surfaces and that's how the virus gets in. To stop the virus from getting to your cells you want the antibodies at the point at which it's meeting your cells so you can block it," she said. Dr Enjuanes said his inhalable vaccine creates “a sterilising immunity, meaning there is no possibility for the virus to replicate”. Dr Enjuanes believes that the unique process his team is using will make their product “the most powerful”, claiming that the single-dose spray will offer “100 per cent protection” and pointing to good results so far in tests on mice. However, it will take time to get it to the market, he said. “Because our system is completely new, the regulatory agencies will be asking for many more controls. That’s the reason we’ll be a little bit later, assuming we are lucky and there are no negative side-effects when we start testing on humans,” said Dr Enjuanes.

|
Scooped by
Juan Lama
|
A slew of detailed studies has now quantified the increased risk the virus poses to older people, men, and other groups. For every 1,000 people infected with the coronavirus who are under the age of 50, almost none will die. For people in their fifties and early sixties, about five will die — more men than women. The risk then climbs steeply as the years accrue. For every 1,000 people in their mid-seventies or older who are infected, around 116 will die. These are the stark statistics obtained by some of the first detailed studies into the mortality risk for COVID-19. Trends in coronavirus deaths by age have been clear since early in the pandemic. Research teams looking at the presence of antibodies against SARS-CoV-2 in people in the general population — in Spain, England, Italy and Geneva in Switzerland — have now quantified that risk, says Marm Kilpatrick, an infectious-disease researcher at the University of California, Santa Cruz. “It gives us a much sharper tool when asking what the impact might be on a certain population that has a certain demographic,” says Kilpatrick. The studies reveal that age is by far the strongest predictor of an infected person’s risk of dying — a metric known as the infection fatality ratio (IFR), which is the proportion of people infected with the virus, including those who didn’t get tested or show symptoms, who will die as a result. “COVID-19 is not just hazardous for elderly people, it is extremely dangerous for people in their mid-fifties, sixties and seventies,” says Andrew Levin, an economist at Dartmouth College in Hanover, New Hampshire, who has estimated that getting COVID-19 is more than 50 times more likely to be fatal for a 60-year-old than is driving a car. But “age cannot explain everything”, says Henrik Salje, an infectious-disease epidemiologist at the University of Cambridge, UK. Gender is also a strong risk factor, with men almost twice more likely to die from the coronavirus than women. And differences between countries in the fatality estimates for older age groups suggest that the risk of dying from coronavirus is also linked to underlying health conditions, the capacity of health-care systems, and whether the virus has spread among people living in elderly-care facilities. To estimate the mortality risk by age, researchers used data from antibody-prevalence studies. In June and July, thousands of people across England received a pinprick antibody test in the post. Of the 109,000 randomly selected teenagers and adults who took the test, some 6% harboured antibodies against SARS-CoV-2. This result was used to calculate an overall IFR for England of 0.9% — or 9 deaths in every 1,000 cases. The IFR was close to zero for people between the ages of 15 and 44, increasing to 3.1% for 65–74-year-olds and to 11.6% for anyone older. The results of the study have been posted to the medRxiv preprint server. Another study from Spain that started in April, and tested for antibodies in more than 61,000 residents in randomly selected households, observed a similar trend. The overall IFR for the population was about 0.8%, but it remained close to zero for people under 50, before rising swiftly to 11.6% for men 80 years old and over; it was 4.6% for women in that age group. The results also revealed that men are more likely to die of the infection than are women — the gap increasing with age. “Men face twice the risk of women,” says Beatriz Pérez-Gómez, an epidemiologist at the Carlos III Institute of Health in Madrid, who was involved in the Spanish study. The results have also been posted to the medRxiv server.Differences in the male and female immune-system response could explain the divergent risks, says Jessica Metcalf, a demographer at Princeton University, New Jersey. “The female immune system might have an edge by detecting pathogens just a bit earlier,” she says...

|
Scooped by
Juan Lama
|
MADRID - Spain aims to roll out a COVID-19 contact-tracing app across the country in September after saying on Monday that a pilot showed it could detect almost twice as many potential infections as human trackers during a simulated outbreak on a tiny island. In the absence of a vaccine or cure, states are deploying Bluetooth wireless technology to log contacts and alert people when someone they have been near tests positive. Spain used a new system developed by Google <GOOGL.O> and Apple <AAPL.O> which holds data on individual devices to ensure privacy, to build an app it tested on La Gomera, an island next to the tourist hotspot of Tenerife in the Canary archipelago, in July. Now the government aims to offer it to regional health authorities who could have it ready by mid-September, and from Aug. 10 to tourism-dependent areas or places where cases are rising, said Carme Artigas, head of the state digital and artificial intelligence unit. "The app sees more than we see because we only remember contacts with people we know, but the app also remembers contacts with strangers," Artigas said. "It is anonymous and much less intrusive than receiving a call from someone who wants to reconstruct everything you have done for the past 15 days," Artigas added.
Some 3,200 people downloaded the app, just pipping a target of 3,000. Participants anonymously entered randomly distributed codes into the app, some of which falsely indicated a positive COVID-19 test, which then alerted everyone with whom they had spent a minimum of 15 minutes at a proximity of 2 metres (6.5 ft) or less. For every virtual positive diagnosis, the app identified an average 6.4 contacts with others, Artigas's ministry said in a statement, compared with an average 3.5 contacts identified by human tracers in the Canary Islands. The spread of the disease in Spain slowed as the government imposed one of the strictest lockdowns in Europe and as many countries limited international travel, but new cases have started rising again, hitting a post-lockdown record of 1,525 on Friday.

|
Scooped by
Juan Lama
|
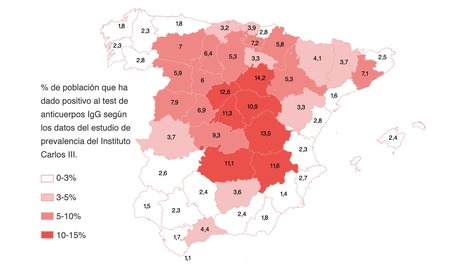
Spain is one of the European countries most affected by the COVID-19 pandemic. Serological surveys are a valuable tool to assess the extent of the epidemic, given the existence of asymptomatic cases and little access to diagnostic tests. This nationwide population-based study aims to estimate the seroprevalence of SARS-CoV-2 infection in Spain at national and regional level. 35,883 households were selected from municipal rolls using two-stage random sampling stratified by province and municipality size, with all residents invited to participate. From April 27 to May 11, 2020, 61 075 participants (75·1% of all contacted individuals within selected households) answered a questionnaire on history of symptoms compatible with COVID-19 and risk factors, received a point-of-care antibody test, and, if agreed, donated a blood sample for additional testing with a chemiluminescent microparticle immunoassay. Prevalences of IgG antibodies were adjusted using sampling weights and post-stratification to allow for differences in non-response rates based on age group, sex, and census-tract income. Using results for both tests, we calculated a seroprevalence range maximizing either specificity (positive for both tests) or sensitivity (positive for either test). Seroprevalence was 5·0% (95% CI 4·7–5·4) by the point-of-care test and 4·6% (4·3–5·0) by immunoassay, with a specificity–sensitivity range of 3·7% (3·3–4·0; both tests positive) to 6·2% (5·8–6·6; either test positive), with no differences by sex and lower seroprevalence in children younger than 10 years (<3·1% by the point-of-care test). There was substantial geographical variability, with higher prevalence around Madrid (>10%) and lower in coastal areas (<3%). Seroprevalence among 195 participants with positive PCR more than 14 days before the study visit ranged from 87·6% (81·1–92·1; both tests positive) to 91·8% (86·3–95·3; either test positive). In 7273 individuals with anosmia or at least three symptoms, seroprevalence ranged from 15·3% (13·8–16·8) to 19·3% (17·7–21·0). Around a third of seropositive participants were asymptomatic, ranging from 21·9% (19·1–24·9) to 35·8% (33·1–38·5). Only 19·5% (16·3–23·2) of symptomatic participants who were seropositive by both the point-of-care test and immunoassay reported a previous PCR test. The majority of the Spanish population is seronegative to SARS-CoV-2 infection, even in hotspot areas. Most PCR-confirmed cases have detectable antibodies, but a substantial proportion of people with symptoms compatible with COVID-19 did not have a PCR test and at least a third of infections determined by serology were asymptomatic. These results emphasize the need for maintaining public health measures to avoid a new epidemic wave. Published in The Lancet (July 6, 2020): https://doi.org/10.1016/S0140-6736(20)31483-5

|
Scooped by
Juan Lama
|
Only 5% of Spaniards have been infected with the coronavirus, according to preliminary data released of the seroprevalence study performed by the Instituto de Salud Carlos III, which tested near 70,000 participants. Infection rates show great geographic variation with some provinces having a prevalence seven times higher than others. Soria is the area with the highest percentage of people exposed to the disease, 14.2%. In Madrid the prevalence is 11.3%. Another conclusion from the preliminary report presented this afternoon is that more than 90% of the infections occurred in Spain were not detected by the health system. The country's official statistics reported 228,691 confirmed PCR-positive cases, but according to the preliminary data 2,350,000 people have been exposed to the disease, many without even noticing it. With 27,100 deaths reported in the country, the case fatality is estimated between 1 and 1.2% ", according to Jesús Molina Cabrillana, epidemiologist at the Spanish Society of Preventive Medicine, Public Health and Hygiene. Near one in three (33.7%) of the seropositive population had asymptomatic infections and passed the disease without noticing. Eight percent of the population with antibodies self-reported three or four symptoms, 14.7% more than five symptoms and 43% reported sudden loss of smell (anosmia). See also Study in the Lancet (July 6, 2020): https://doi.org/10.1016/S0140-6736(20)31483-5

|
Scooped by
Juan Lama
|
We would like to express our concern about the limited capacity of actions taken by the Spanish Government to successfully control the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) outbreak and end the exponential growth phase of new cases. The measures taken so far, consisting primarily of partial restriction mobility, are in the right direction, although some researchers have warned about the pressure placed on the building blocks of the health system. Given that the actual extent of an epidemic can only be assessed retrospectively, governments and policy makers are forced to make decisions on the basis of mathematical models of other diseases and previous experiences by other countries taking different actions. In Spain, various models simulating the spread of infection and using different assumptions converge in a landscape of a high number of new cases within the next few weeks. Simulations have been done using the URV and UNIZAR models to predict the progression of the number of patients who will require admission into hospital intensive care units because of coronavirus disease 2019 (COVID-19) in three scenarios (appendix): scenario 1, no mobility restrictions; scenario 2, partial restriction of mobility (ie, movement to the workplace allowed for 30% of people); and scenario 3, complete restriction of mobility (ie, no workplace mobility allowed except for essential services). The model suggests that the actions taken to date, consistent with scenario 2, will be insufficient to prevent hospitals and intensive care units from being overwhelmed over the coming weeks. The foreseen collapse of the health system, along with the age distribution of the Spanish population (ie, 18% of people aged ≥65 years), suggests a potentially high mortality rate associated with COVID-19 in the country.... Published in The Lancet (March 26, 2020): https://doi.org/10.1016/ S0140-6736(20)30753-4
|

|
Scooped by
Juan Lama
|
The COVID-19 pandemic has sparked extensive discussions about its effect on mental health. While global suicide rates remained stable during the pandemic, the specific impact on non-lethal suicidal behaviors, namely, ideation or suicide attempts that are survived, during and after the pandemic had not been explored. A new study, led by Dr. Víctor Serrano-Gimeno from the Mental Health Research Group of the Sant Pau Research Institute (IR Sant Pau), reveals a significant increase in these behaviors after the lockdown. The study, published in The Lancet Psychiatry, analyzes data from a Catalan cohort from all hospitals in Catalonia collected through the Catalan Suicide Risk Code in three periods: the pre-lockdown period (January 1, 2018, until the implementation of the lockdown in Spain on March 14, 2020); the lockdown period (March 14, 2020, until the end of the lockdown on June 21, 2020); and the post-lockdown period (June 21, 2020, until December 31, 2022). The results reveal a slight increasing trend in non-lethal suicidal behaviors from January 1, 2018, until March 13, 2020, followed by a reduction during the lockdown period and a 50.77% increase after the lockdown measures. These results highlight the prolonged impact of the pandemic on the population's mental health. Dr. Serrano-Gimeno explains that "this study provides a comprehensive examination of non-lethal suicidal behaviors in Catalonia, highlighting the dynamics of the different phases of the COVID-19 pandemic. "The initial reduction during the strict quarantine may be explained because people have less access to methods of suicide, among other reasons. And the subsequent increase after the lockdown reflects complex factors, including social isolation and economic challenges." Specifically, stratified data analyses indicated that the relaxation of the lockdown resulted in a significant increase in non-lethal suicidal behaviors among women—especially in the 18 to 30 age group—and among minors under 18. These results underscore the need for preventive strategies targeted at these groups. Dr. Maria Portella, head of the Mental Health Research Group at IR Sant Pau, emphasizes the importance of this study because "it quantifies what we already suspected about mental health during the pandemic. It highlights the need for a perspective beyond mental illness to address suicidality, addressing it as a fundamental aspect of public health." For her, "this article highlights the much longer-term consequences of the decisions made during the pandemic. We quantify it, but it also puts a much broader focus on mental health in the sense that it wasn't necessarily people with a psychiatric diagnosis. And this is very important because it shows that suicide is a much more global public health issue." In this regard, Dr. Narcís Cardoner, researcher from the Mental Health Research Group at IR Sant Pau and head of the Psychiatry Department at Sant Pau Hospital, adds that these results tell us many things that should be used to face similar situations better in the future. "It's interesting that throughout the pandemic, physical health was markedly prioritized. And all strategies, for example, the lockdown itself, were aimed at reducing the risk of people getting infected with the virus. But we knew that the impact of these situations would go beyond. And there's always talk of a fourth wave, which is the mental health problem. And it seems that we were somewhat oblivious to this situation. "Data like those derived from this study say that physical health is very important, but there is no health without mental health, and it would have been essential to have made some provision for these impacts." He also emphasized that "sometimes what's good for physical health isn't always good for mental health. So here, looking to the future, we must propose more holistic approaches to similar situations. I think it's an important lesson from what happened with the pandemic, especially considering that it mainly affected young women and minors. It's a lesson whose effects we knew, we were aware of, but we were absolutely turning our backs on it. We somewhat overlooked it or denied it." In fact, the three experts agree that during the pandemic, other countries had more lenient lockdown measures "that seemed to not have a differentiated impact in the field of physical health, and we don't know why because it's true that mental health data seem to be quite generalizable worldwide."The impact of the pandemic, for example, in terms of the risk of depression, anxiety disorders, has been very marked worldwide. Rates, the prevalence of depression, and anxiety have increased. So, we're identifying a very generalizable phenomenon." For them, it's necessary that in future occasions much more global measures are considered "and to think of mental health as an essential part of health. Since the effects are not so immediate, perhaps we think they're like second-level issues, as if they weren't so important." Finally, Dr. Cardoner emphasizes the current pressure on the health care system, "You just have to go through our emergency rooms to see the saturation. This demonstrates that the pandemic has been a brutal stress test for an already fragile society. This study is important because it quantifies it. We all had this idea that mental health was doing terribly. And here we can confirm it with numbers. the situation has evolved as it has evolved." Dr. Serrano concludes that "the results show us that the consequences of large-scale social phenomena are profound, and this must be addressed from a public health perspective, not just psychiatry." Study cited published in The Lancet Psychaiatry (May 2024): https://doi.org/10.1016/S2215-0366(24)00065-8

|
Scooped by
Juan Lama
|
In October 2022, an outbreak in Europe of highly pathogenic avian influenza (HPAI) A(H5N1) in intensively farmed minks occurred in northwest Spain. A single mink farm hosting more than 50,000 minks was involved. The identified viruses belong to clade 2.3.4.4b, which is responsible of the ongoing epizootic in Europe. An uncommon mutation (T271A) in the PB2 gene with potential public health implications was found. Our investigations indicate onward mink transmission of the virus may have occurred in the affected farm. Published in Eurosurveillance (Jan. 18, 2023): https://doi.org/10.2807/1560-7917.ES.2023.28.3.2300001

|
Scooped by
Juan Lama
|
BARCELONA, Spain (AP) — Spain reported Saturday a second death in as many days from monkeypox. These are believed to be the first confirmed fatalities from the disease in Europe since its recent spread beyond Africa. The ministry based in Madrid said both fatalities were young men. It reported its first death on Friday, the same day that Brazil also reported its first death from monkeypox. The global monkeypox outbreak has seen more than 22,000 cases in nearly 80 countries since May. There have been 75 suspected deaths in Africa, mostly in Nigeria and Congo, where a more lethal form of monkeypox is spreading than in the West. In the U.S. and Europe, the vast majority of monkeypox infections have happened in men who have sex with men, though health officials have stressed that anyone can catch the virus. The deaths outside Africa come one week after the World Health Organization declared the monkeypox outbreak a global health emergency. “The notification of deaths due to monkeypox does not change our assessment of the outbreak in Europe. We know that although the disease is self-limiting in most cases, monkeypox can cause severe complications,” said Catherine Smallwood, Senior Emergency Officer at WHO Europe. “With the continued spread of monkeypox in Europe, we will expect to see more deaths. Our goal needs to be on interrupting transmission quickly in Europe and stopping this outbreak,” she said. On Friday, Spain’s health ministry reported 4,298 people were infected with the virus, making it the leading European country for monkeypox cases. Of that total, some 3,500 cases were of men who had had sex with other men. Only 64 were women. The ministry said 120 have needed hospital attention. Smallwood said around 8% of the monkeypox cases in Europe have required hospitalization. Monkeypox has been endemic to parts of Africa for decades. Its leap to Europe and North America was linked by experts to two raves in Belgium and Spain. Spanish health authorities are administering 5,300 vaccines that Spain received from the joint EU vaccine purchase scheme. Health workers say that’s far fewer than the number needed to cover the at-risk groups. But the rush to buy limited vaccines by richer Western countries is putting Africa in danger of being left out. Monkeypox spreads mainly through skin-to-skin contact, but it can also be transmitted through bed sheets used by someone with monkeypox. Symptoms include fever, body aches, chills, fatigue and hives. The illness has been relatively mild in many men. But people can be contagious for weeks, and the lesions can be extremely painful. AP Medical Writer Maria Cheng contributed to this report from London.

|
Scooped by
Juan Lama
|
Two people have died in Japan days after receiving doses from a batch of Moderna Covid-19 vaccines whose use was suspended Thursday following concerns over a contamination risk, the country's Ministry of Health, Labor and Welfare said Saturday. A causal link between the vaccine and the deaths has not yet been established, according to the ministry and Takeda Pharmaceutical Company, which distributes the Moderna vaccine in Japan. Japan suspended the use of about 1.63 million doses of the Moderna vaccine on August 26 as a precaution after foreign substances were found in some vials. While inquiries are being conducted by the Japanese government and three pharmaceutical companies involved, no police investigation has been announced and there is no present indication of wrongdoing. "Currently, no link has been confirmed between these deaths and the Moderna vaccine, but we believe it is important to carry out a formal probe to investigate the matter further," Takeda Pharmaceutical Company said in a statement released Saturday. Japan's Ministry of Health will conduct that investigation alongside Takeda, the company stated, adding that Moderna has its own investigation underway. Rovi, a Spanish company that manufactured the batches, described the contaminant as "particulate matter" in a statement Thursday. Rovi said it is also investigating the contaminated lots. The 1.63 million doses came from three identified lot numbers -- 3004667, 3004734 and 3004956. The doses had been distributed to 863 vaccination sites across Japan, and some were used. The health ministry said it began notifying the vaccination sites on Thursday morning about the contamination risk. The two people who died had received vaccines from lot 3004734, one of the lots removed from circulation Thursday. Japan's Ministry of Health, Labor and Welfare said that no foreign contaminants had been reported from this lot yet. Results from laboratory tests from contaminated samples will be available in the coming days, according to Takeda. CNN has reached out to Moderna for comment.

|
Scooped by
Juan Lama
|
The World Health Organization (WHO) has warned that coronavirus cases are surging alarmingly in Europe, as a "very serious situation" unfolds across the continent. As Covid-19 infections spike to record numbers, European governments are imposing strict local measures and weighing up further lockdowns in a bid to halt a second wave of the pandemic. But WHO regional director Hans Kluge said at a Thursday news conference that the increase in cases should serve as a warning of what is to come. "Weekly cases have now exceeded those reported when the pandemic first peaked in Europe in March," Kluge said. "Last week, the region's weekly tally exceeded 300,000 patients." More than half of European nations have reported an increase of more than 10% in new cases in the past two weeks, Kluge added. "Of those, seven countries have seen newly reported cases increase more than two-fold in the same period," he said. "In the spring and early summer we were able to see the impact of strict lockdown measures. Our efforts, our sacrifices, paid off. In June cases hit an all-time low. The September case numbers, however, should serve as a wake-up call for all of us," he said. "Although these numbers reflect more comprehensive testing, it also shows alarming rates of transmission across the region." While there was an increase in cases in older age groups, those aged 50 to 79, in the first week of September, Kluge said, the biggest proportion of new cases is still among 25- to 49-year-olds. Countries across the continent have been easing lockdowns and reopening their economies, but governments are now scrambling to avert further outbreaks. "This pandemic has taken so much from us," Kluge said, citing the nearly 4.9 million recorded Covid-19 cases in Europe and more than 226,000 deaths. "And this tells only part of the story," he said. "The impact on our mental health, economies, livelihoods and society has been monumental." In France, Covid-19 hospitalizations have risen in recent days in large cities such as Paris, Bordeaux and Marseille. Earlier this year, the first coronavirus wave spiked fast in France, but it was cut short by a strict nationwide lockdown. In total more than 31,000 people died there from the disease, out of more than 443,000 cases, according to Johns Hopkins University (JHU). Now, the number of new infections is rising fast. A record was set over the weekend with more than 10,000 new cases in a single day. The number of clusters has been rising steadily and, most worryingly, nationwide, the number of people in intensive care has risen 25% in the past week. Cases in the United Kingdom, Germany, Spain and Italy have also increased. New restrictions were imposed across England this week barring people from meeting socially in groups of more than six, of all ages, indoors or outdoors. Scotland and Wales have also tightened their social distancing rules. From Friday, even stricter measures will apply in the northeast of England amid a "concerning rise" in Covid-19 infection rates there, UK Health Secretary Matt Hancock announced in Parliament on Thursday. The measures include a ban on socializing outside households or "support bubbles" and a mandated closing time of 10 p.m. for all bars, pubs, restaurants and leisure centers. They will apply to seven areas -- including the cities of Newcastle, Sunderland and Durham -- and will affect more than 1.5 million people. Hancock stressed the need to take "immediate action" against the virus with winter approaching. At least 41,773 people have died with coronavirus in the UK, according to JHU, the highest toll in Europe and fifth-largest number of any country in the world. The UK government has come under pressure over recent failings in its coronavirus testing system, with some people -- including health care workers -- experiencing difficulty in accessing tests or being directed to testing sites far from home. Prime Minister Boris Johnson defended Britain's coronavirus testing record Wednesday, saying it compared favorably to other European countries and that recent problems were due to a "colossal spike" in demand...

|
Scooped by
Juan Lama
|
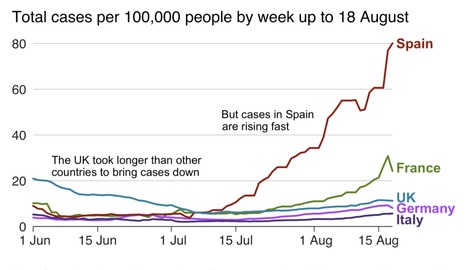
Spain saw one of the most draconian Covid-19 lockdowns in Europe, but two months after it was lifted, the virus is spreading faster than in any neighbouring nation. It now has Europe's fastest-rising caseload, with 142 positive cases per 100,000 inhabitants over the past two weeks. By the time the state of emergency ended on 21 June, Spain was registering 100 to 150 cases per day. That number has risen to more than 3,000. But the number of deaths over the past week stood at 122 on Thursday, a far cry from the 950 registered on 2 April alone, the blackest day in Europe's deadliest per capita coronavirus epidemic. Most of the transmission is now between young people, and around three-quarters of positives are in patients who show no symptoms. Spain's government admits the numbers are "not what we want to see", but points to key differences compared to the spring. Only around 3% of current cases require hospital treatment, less than 0.5% need intensive care and the current death rate is as low as 0.3%. "Mortality is very low, as is the hospitalisation rate. Something has changed big time, although the rise is still worrying," says Ildefonso Hernández, a professor in public health from Miguel Hernández University in Alicante. "As long as cases are rising, we have to think that a second wave is on the way. We don't have much time to react before September's return to routines." Spain's tourism season has ended up as little more than a damp squib, as most countries moved to blacklist this key destination within weeks of the country opening up at the end of June. That means beach areas have so far avoided the highest rates of infection, although Catalonia's infection rate is slightly above the national average on 145 cases per 100,000 inhabitants. Healthcare is a competence of Spain's 17 regions, and some are looking much better prepared than others. At the good end of the scale, the northern region of Asturias has an infection rate of 32, while Aragón in the north-east is topping 500. Aragón's capital, Zaragoza, has become a hotspot for community transmission over recent weeks, but the problems began in the early summer when thousands of seasonal workers, many of them wandering migrants, began to travel to orchards in the region. Growers and packing companies have been criticised for not providing accommodation for migrant workers, leading them to travel between shelters and fields or subsist in insanitary shanties. "Everything happening in Aragón is very much connected to outbreaks among the seasonal fruit-pickers. There should have been more anticipation of the problems that could arise due to the accommodation situation of these workers," explains Juan González Armengol, president of the Spanish Society of Emergency Medicine (Semes). Worst of all, more than 55 care homes for the elderly in Aragón have registered cases since the end of the state of emergency..

|
Scooped by
Juan Lama
|
Agriculture minister says origins of outbreak unclear after seven farm workers – and 87% of the mink – test positive. Spain has ordered the culling of nearly 100,000 mink on a farm after confirming many were carrying coronavirus, a regional minister said on Thursday. Joaquin Olona, agriculture minister for the north-eastern Aragon region, said the cull would involve the slaughter of 92,700 mink which are prized for their pelt. Officials suspect the virus first reached the farm through a worker who passed it on to the animals. But Olona said it was not completely clear if “transmission was possible from animals to humans and vice versa”. In the Netherlands tens of thousands of mink have been slaughtered since the start of the pandemic after 20 farms were found to be infected, the Dutch authorities said earlier this month. The move came after at least two farm workers were found to be infected in May, most likely by the mink, with the World Health Organization saying it could be the first known cases of animal-to-human transmission. In Spain the mink farm – in Puebla de Valverde, about 100km (60 miles) north-west of the coastal resort of Valencia – has been carefully monitored since 22 May after seven workers tested positive for Covid-19, Olona said. Since then no animals have left the property, which is the only mink farm in Aragon. Officials have since carried out a string of PCR tests which on 13 July showed that 87% of the mink were infected, prompting the decision to carry out a cull “to avoid the risk of human transmission”, Olona said....

|
Scooped by
Juan Lama
|
Scientists not involved in the study seriously doubt the findings, which challenge the current consensus on where and when the virus originated. In a study not yet published in a journal, scientists have reported that the new coronavirus was present in wastewater in Barcelona, Spain in March 2019, a finding that, if confirmed, would show that the pathogen had emerged much earlier than previously thought. But independent experts who reviewed the findings said they doubted the claim. The study was flawed, they said, and other lines of evidence strongly suggest the virus emerged in China late last year. Up until now, the earliest evidence of the virus anywhere in the world has been from December 2019 in China and it was only known to have hit mainland Spain in February 2020. “Barcelona is a city that is frequented by Chinese people, in tourism and business, so probably this happened also elsewhere, and probably at the same time,” said the lead author, Albert Bosch, a professor in the Department of Microbiology of the University of Barcelona who has been studying viruses in wastewater for more than 40 years. Several experts not involved in the research pointed out problems with the new study, which has not yet been subjected to the critical review by outside experts that occurs before publication in a scientific journal. They suggested that the tests might very well have produced false positives because of contamination or improper storage of the samples. “I don’t trust the results,” said Irene Xagoraraki, an environmental engineer at Michigan State University. Researchers at the University of Barcelona posted their findings online on June 13. Most of their report described research on wastewater treatments from early 2020. Preprint available at medRxiv (June 13, 2020): https://doi.org/10.1101/2020.06.13.20129627

|
Scooped by
Juan Lama
|
Health care workers (HCW) are a high-risk population to acquire SARS-CoV-2 infection from patients or other fellow HCW. At the same time, they can be contagious to highly vulnerable individuals seeking health care. This study aims at estimating the seroprevalence of antibodies against SARS-CoV-2 and associated factors in HCW from a large referral hospital in Barcelona, Spain, one of the countries hardest hit by COVID-19 in the world. From 28 March to 9 April 2020, we recruited a random sample of 578 HCW from the human resources database of Hospital Clínic in Barcelona. We collected a nasopharyngeal swab for direct SARS-CoV-2 detection through real time reverse-transcriptase polymerase chain reaction (rRT-PCR), as well as blood for plasma antibody quantification. IgM, IgG and IgA antibodies to the receptor-binding domain of the spike protein were measured by Luminex. The cumulative prevalence of infection (past or current) was defined by a positive SARS-CoV-2 rRT-PCR and/or antibody seropositivity. Of the 578 total participants, 39 (6.7%, 95% CI: 4.8-9.1) had been previously diagnosed with COVID-19 by rRT-PCR, 14 (2.4%, 95% CI: 1.4-4.3) had a positive rRT-PCR at recruitment, and 54 (9.3%, 95% CI: 7.2-12.0) were seropositive for IgM and/or IgG and/or IgA against SARSCoV-2. Of the 54 seropositive HCW, 21 (38.9%) had not been previously diagnosed with COVID-19, although 10 of them (47.6%) reported past COVID-19-compatible symptoms. The cumulative prevalence of SARS-CoV-2 infection was 11.2% (65/578, 95% CI: 8.9-14.1). Among those with evidence of past or current infection, 40.0% (26/65) had not been previously diagnosed with COVID-19, of which 46.2% (12/26) had history of COVID-19-compatible symptoms. The odds of being seropositive was higher in participants who reported any COVID19 symptom (OR: 8.84, 95% CI: 4.41-17.73). IgM levels positively correlated with age (rho=0.36, p-value=0.031) and were higher in participants with more than 10 days since onset of symptoms (p-value=0.022), and IgA levels were higher in symptomatic than asymptomatic subjects (p-value=0.041). The seroprevalence of antibodies against SARS-CoV-2 among HCW was lower than expected. Thus, being a high-risk population, we anticipate these estimates to be an upper limit to the seroprevalence of the general population. Forty per cent of those with past or present infection had not been previously diagnosed with COVID-19, which calls for active periodic rRT-PCR testing among all HCW to minimize potential risk of hospital-acquired SARS-CoV-2 infections. In summary, we found that 9.3% (95% CI: 7.2-12.0) of HCW from a large Spanish referral hospital (recruited from March 28th to April 9th, 2020) developed detectable IgA, IgG and/or IgM antibodies. Given that HCW are a high risk population for SARS-CoV-2, it is likely that the community seroprevalence is lower than this figure, showing that we are still very far from reaching the 67% herd immunity level that is estimated to be needed to protect the susceptible population,23 assuming that this immunity prevents from reinfection.

|
Scooped by
Juan Lama
|
Spanish health authorities have confirmed a case of a man spreading dengue through sex, a world first for a virus which until recently was thought to be transmitted only by mosquitos. The case concerns a 41-year-old man from Madrid who contracted dengue after having sex with his male partner who picked up the virus from a mosquito bite during a trip to Cuba, said Susana Jimenez of the Madrid region's public health department. His dengue infection was confirmed in September and it puzzled doctors because he had not travelled to a country where the disease, which causes severe flu-like symptoms such as high fever and body aches, is common, she added. "His partner presented the same symptoms as him but lighter around ten days earlier, and he had previously visited Cuba and the Dominican Republic," she said. "An analysis of their sperm was carried out and it revealed that not only did they have dengue but that it was exactly the same virus which circulates in Cuba." A "likely' case of sexual transmission of dengue between a man and a woman was the subject of a recent scientific article in South Korea, she said. In an e-mail sent to AFP, the Stockholm-based European Centre for Disease Prevention and Control (ECDC), which monitors health and disease in Europe, said this was "to our knowledge, the first sexual transmission of the dengue virus among men who have sex with men." Dengue is transmitted mainly by the Aedes Aegypti mosquito, which thrives in densely-populated tropical climates and breeds in stagnant pools of water. It kills 10,000 people a year and infects over 100 million. The disease is fatal only in extreme cases but the symptoms are extremely unpleasant, including a high fever, severe headaches and vomiting. It also exacts a heavy economic burden on countries as sufferers are unable to work, as well as overwhelming health services when there is a severe outbreak. It is most serious - and deadly - in children, especially young girls. Scientists do not know why. Dengue is most commonly caught by people traveling to hotter climates such as South East Asia, Africa, Australia, the Caribbean and South and Central America.
|



 Your new post is loading...
Your new post is loading...