Understanding the death toll — who makes up the one million and how the country failed them — is essential as the pandemic continues.
Get Started for FREE
Sign up with Facebook Sign up with X
I don't have a Facebook or a X account

 Your new post is loading... Your new post is loading...
From
www
It's the highest total in the world - but the WHO thinks the true death toll may be higher elsewhere.
The US has passed more than one million Covid-related deaths, says the White House.
President Joe Biden said the country was marking "a tragic milestone" and each death was "an irreplaceable loss". It's the highest official total in the world - although the World Health Organization believes the true death toll may be much higher elsewhere. The US has also recorded more than 80 million Covid cases, out of a 330 million population. The first confirmed case was reported on 20 January 2020, when a man flew home to Seattle from Wuhan in China. The 35-year-old survived, after 10 days of pneumonia, coughs, fever, nausea and vomiting. But deaths began to be reported just a few weeks later. In the two years since, death rates have ebbed and flowed as waves of the virus swept across the country - reaching highs of more than 4,000 a day in early 2021. Public health experts give several reasons for the high US death toll - including high rates of obesity and hypertension, overworked hospital systems, some vaccine hesitancy and a large older population. Each US state may have a slightly different way to define a Covid death, and such deaths are often not solely because of the virus. "One million Covid deaths, one million empty chairs around the family dinner table, each irreplaceable losses," said President Biden in a televised statement on Thursday morning. "Our heart goes out to all those who are struggling, asking themselves, how do we go on without him, how do we go on without her?" The president ordered the White House flags to be lowered to half mast to mark the milestone. When did the deaths take place?The US has seen the number of daily reported deaths spike on several occasions, often coming as new variants spread across the country. The first wave - the initial pandemic - saw highs of more than 2,500 daily reported deaths in April 2020, about eight months before the first vaccines were rolled out in December. "The dangerous surges, where our hospitals were full and new deaths were overwhelming, have all come on the heels of new variants," Dr Mark Cameron, an associate professor in the department of population and quantitative health sciences at Case Western University in Ohio, told the BBC. Most of the one million Americans who died during the pandemic lost their lives after the vaccines were introduced. That's down to the sheer scale of people still catching the virus - it does not mean the vaccines aren't working. Vaccines massively cut severe Covid risk. A study from the Rand Corporation credited the jabs with saving 140,000 lives in the US by May 2021 alone. A separate analysis by the Peterson Center for Healthcare and the Kaiser Family Foundation in April this year estimated that around a quarter of the US deaths - about 234,000 people - could have been prevented with vaccines. "You can't necessarily simplify this to be a pandemic of the unvaccinated. Everyone knows someone who had the whole vaccination regimen and still got very sick," Dr Cameron added. "But the data is clear, the risk of Covid-19 and death is higher in the unvaccinated." Where in the US did the deaths take place?Of the 50 US states, the highest death toll has been reported in California, where about 90,000 people have died. California is followed closely by Texas (about 86,000), Florida (about 74,000) and New York (about 68,000). On a per capita basis, CDC data shows that Mississippi has suffered about 418 deaths per 100,000 residents, followed by Arizona (414), Alabama (399) and West Virginia (384). The per capita death rate in these states far surpasses the average US national rate of about 300 per 100,000. Experts point to several reasons why certain states suffered disproportionately, including unequal access to healthcare. Brittany Kmush, an epidemiologist and global health expert at Syracuse University, said socio-economic status often affected "being able to access hospitals with oxygen and things like that when patients need them". Dr Monica Gandhi, an infectious diseases physician and professor at the University of California San Francisco, said vaccine hesitancy also explains higher death tolls in certain states. In her analysis, shortcomings in vaccinations have contributed more to the US death toll than other public health measures, such as masking or isolation. Demographic trendsWhile deaths have been reported across all age and ethnic groups, experts note that certain sectors of the population have been more likely to die - particularly the elderly and those with co-morbidities. Government data shows the vast majority of Covid deaths in the US - about 740,000 - have been among those older than 65. "Looking at severe illness and death, the demographics haven't changed throughout the pandemic. It has always been older adults, and those with co-morbidities especially," Dr Cameron explained. CDC data analysed by the Kaiser Family Foundation shows that overall - particularly in the early stages of the pandemic in 2020 - black, Hispanic and Native American populations experienced higher rates of both infection and death. Public health experts cite a range of reasons, including vaccine hesitancy among some groups, and an elevated risk of exposure due to working and living conditions. "Part of that is being unable to separate yourself from work," Dr Gandhi said. "And even after the vaccine, there was some scepticism in some of our black and Hispanic populations about taking up the vaccine. But there was a lot more acceptance after Delta. That really scared people." The true toll?While the death toll from Covid-19 now officially exceeds one million, the indirect toll of the virus is likely to be far higher, as a result of disrupted health systems and a hesitancy to seek medical attention for fear of catching the virus. One study, published in the journal PLOS Medicine in May 2021, found that for every 100 deaths directly assigned to Covid, another 20 "excess" deaths occurred that were not - many of them in areas with "lower socio-economic status". A study released on Thursday by the World Health Organization put the figure at 140 excess deaths per 100,000 people during 2020 and 2021 - totalling about 930,000 more lives lost than would have been expected on average. "People were waiting for surgery and not seeing their doctors, and [there were] missed opportunities for serious disease diagnoses," Dr Cameron said, adding that this was particularly true for those aged between 25 and 64. "It will be years before we even come close to understanding the impact Covid-19 had on our overall morbidity and mortality rates."
From
apnews
Nearly all COVID-19 deaths in the U.S. now are in people who weren’t vaccinated, a staggering demonstration of how effective the shots have been and an indication that deaths per day — now down to under 300 — could be practically zero if everyone eligible got the vaccine. An Associated Press analysis of available government data from May shows that “breakthrough” infections in fully vaccinated people accounted for fewer than 1,200 of more than 853,000 COVID-19 hospitalizations. That’s about 0.1%. And only about 150 of the more than 18,000 COVID-19 deaths in May were in fully vaccinated people. That translates to about 0.8%, or five deaths per day on average. The AP analyzed figures provided by the Centers for Disease Control and Prevention. The CDC itself has not estimated what percentage of hospitalizations and deaths are in fully vaccinated people, citing limitations in the data. Among them: Only about 45 states report breakthrough infections, and some are more aggressive than others in looking for such cases. So the data probably understates such infections, CDC officials said. Still, the overall trend that emerges from the data echoes what many health care authorities are seeing around the country and what top experts are saying. Earlier this month, Andy Slavitt, a former adviser to the Biden administration on COVID-19, suggested that 98% to 99% of the Americans dying of the coronavirus are unvaccinated. And CDC Director Dr. Rochelle Walensky said on Tuesday that the vaccine is so effective that “nearly every death, especially among adults, due to COVID-19, is, at this point, entirely preventable.” She called such deaths “particularly tragic.” Deaths in the U.S. have plummeted from a peak of more than 3,400 day on average in mid-January, one month into the vaccination drive.
About 63% of all vaccine-eligible Americans — those 12 and older — have received at least one dose, and 53% are fully vaccinated, according to the CDC. While vaccine remains scarce in much of the world, the U.S. supply is so abundant and demand has slumped so dramatically that shots sit unused. Ross Bagne, a 68-year-old small-business owner in Cheyenne, Wyoming, was eligible for the vaccine in early February but didn’t get it. He died June 4, infected and unvaccinated, after spending more than three weeks in the hospital, his lungs filling with fluid. He was unable to swallow because of a stroke. “He never went out, so he didn’t think he would catch it,” said his grieving sister, Karen McKnight. She wondered: “Why take the risk of not getting vaccinated?” The preventable deaths will continue, experts predict, with unvaccinated pockets of the nation experiencing outbreaks in the fall and winter. Ali Mokdad, a professor of health metrics sciences at the University of Washington in Seattle, said modeling suggests the nation will hit 1,000 deaths per day again next year. In Arkansas, which has one of the lowest vaccination rates in the nation, with only about 33% of the population fully protected, cases, hospitalizations and deaths are rising. “It is sad to see someone go to the hospital or die when it can be prevented,” Gov. Asa Hutchinson tweeted as he urged people to get their shots. In Seattle’s King County, the public health department found only three deaths during a recent 60-day period in people who were fully vaccinated. The rest, some 95% of 62 deaths, had had no vaccine or just one shot.
“Those are all somebody’s parents, grandparents, siblings and friends,” said Dr. Mark Del Beccaro, who helps lead a vaccination outreach program in King County. “It’s still a lot of deaths, and they’re preventable deaths.” In the St. Louis area, more than 90% of patients hospitalized with COVID-19 have not been vaccinated, said Dr. Alex Garza, a hospital administrator who directs a metropolitan-area task force on the outbreak. “The majority of them express some regret for not being vaccinated,” Garza said. “That’s a pretty common refrain that we’re hearing from patients with COVID.” The stories of unvaccinated people dying may convince some people they should get the shots, but young adults — the group least likely to be vaccinated — may be motivated more by a desire to protect their loved ones, said David Michaels, an epidemiologist at George Washington University’s school of public health in the nation’s capital. Others need paid time off to get the shots and deal with any side effects, Michaels said. The Occupational Safety and Health Administration this month began requiring health care employers, including hospitals and nursing homes, to provide such time off. But Michaels, who headed OSHA under President Barack Obama, said the agency should have gone further and applied the rule to meat and poultry plants and other food operations as well as other places with workers at risk. Bagne, who lived alone, ran a business helping people incorporate their companies in Wyoming for the tax advantages. He was winding down the business, planning to retire, when he got sick, emailing his sister in April about an illness that had left him dizzy and disoriented. “Whatever it was. That bug took a LOT out of me,” he wrote. As his health deteriorated, a neighbor finally persuaded him to go to the hospital. “Why was the messaging in his state so unclear that he didn’t understand the importance of the vaccine? He was a very bright guy,” his sister said. “I wish he’d gotten the vaccine, and I’m sad he didn’t understand how it could prevent him from getting COVID.” ___ The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Department of Science Education. The AP is solely responsible for all content.
British drugmaker AstraZeneca says it has started Phase 3 trials of its coronavirus vaccine candidate in the United States. The vaccine, AZD 1222, is the third to enter large-scale trials in the United States, after vaccines made by Moderna and Pfizer/BioNTech. The vaccine, developed in partnership with Oxford University, has the backing of the US federal government. Rivals Moderna and Pfizer/BioNTec already have Phase 3 trials under way, also with federal government funding. AstraZeneca said it is "recruiting up to 30,000 adults aged 18 years or over from diverse racial, ethnic and geographic groups who are healthy or have stable underlying medical conditions, including those living with HIV, and who are at increased risk of infection from the SARS-CoV-2 virus." Participants will receive two active or placebo doses, spaced four weeks apart. Currently, Phase 3 trials of AstraZeneca's vaccine are going on in Britain, Brazil and South Africa. Trials are also planned for Japan and Russia. The US trial is funded by the federal government's Biomedical Advanced Development Authority and the National Institute of Allergy and Infectious Diseases, part of the National Institutes of Health. "NIH is committed to supporting several Phase 3 vaccine trials to increase the odds that one or more will be effective in preventing COVID-19 and put us on the road to recovery from this devastating pandemic," said NIH director Dr. Francis Collins said in a statement. "We also know that preventing this disease could require multiple vaccines and we're investing in those that we believe have the greatest potential for success." AstraZenca says it intends to enroll more than 50,000 volunteers globally, including 30,000 in the United States, as well as participants in Latin America, Asia, Europe and Africa. The vaccine, called by its experimental name AZD1222, combines a weakened version of a common cold virus that infects chimpanzees and a protein from the virus that causes Covid-19 to induce an immune response. The vaccine was created by Oxford University before being licensed to AstraZeneca for further development. AstraZeneca said it will work with governments and other organizations to produce billions of doses and create broad and equitable access to the vaccine, once it's authorized. "Recent supply announcements with Russia, South Korea, Japan, China, Latin America and Brazil take the global supply capacity towards three billion doses of the vaccine," AstraZeneca said in a statement. The World Health Organization cautioned countries Monday against rushing to develop coronavirus vaccines and advised taking great care in granting emergency use authorization -- a quicker route to getting a vaccine in wide use than full approval, which can take many months...
Explore hospital bed use, need for intensive care beds, and ventilator use due to COVID-19 based on projected deaths for all 50 US states and District of Columbia.
Vir Biotechnology is conducting a research study for COVID-19 patients who have recovered from this infection. This study is being done to understand how the human body’s immune system responds to CoVID-19, a new coronavirus that can cause serious infection in some people. This information may be used to develop new ways to diagnose or treat this infection.
After a phone call to make sure you are eligible to join the study, you will be asked to share some information about your health. A licensed health care professional will then visit you in the comfort of your own home to draw a blood sample. You will receive an Amazon gift card for participating. You must be between the ages of 18 to 70 years of age and you must have had documented COVID-19 infection. You can still participate even if you have not had symptoms of infection. You must meet other study requirements.
If you are interested and want more information contact email Vir Biotechnology at virus@vir.bio |
As cases rise in the U.S. and other parts of the world, Omicron subvariants are a continued culprit. Experts are watching closely to see if further mutations of the virus may become even more contagious, or may gain the ability to evade immunity from prior infections and vaccinations. BA.4 and BA.5 in South AfricaWhen South African scientists sounded the alarm about Omicron in November, they identified three versions of the variant, called BA.1, BA.2, and BA.3. BA.1 first spread rapidly through South Africa and the rest of the world in December and January; BA.2 then outcompeted BA.1 to become the dominant strain globally. Now, South African scientists are sounding the alarm again: this time about new Omicron lineages, dubbed BA.4 and BA.5. These two lineages have driven another new surge in the country, with both cases and hospital admissions rising sharply in recent weeks. The surge might be starting to slow, as of late this week, but it’s unclear if this trend will continue. South Africa saw a huge BA.1 surge in November and December, then didn’t see much of a BA.2 bump—likely because so many people infected with BA.1 had immunity to this variant. But BA.4 and BA.5 may be a different story, according to a preprint from Alex Sigal and colleagues at the Africa Health Research Institute. Sigal and his collaborators tested neutralizing antibodies—a commonly-studied aspect of immune system protection—from BA.1 against BA.4 and BA.5. They found that a BA.1 infection offered relatively limited protection against BA.4 and BA.5, especially if the person who had BA.1 was unvaccinated. “BA.4 and BA.5 have potential to result in a new infection wave,” the authors wrote. This study is a preprint, not yet peer-reviewed. But it’s still a major warning sign for the U.S. and other countries: watch out for BA.4 and BA.5.
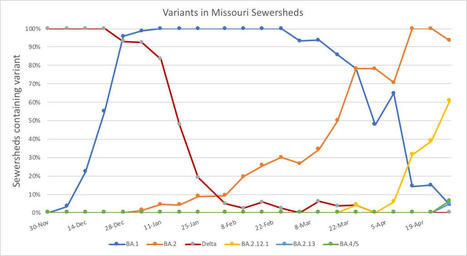
BA.2 subvariants in the U.S.Meanwhile, here in the U.S., BA.2 continues to mutate and spread rapidly. The BA.2.12.1 subvariant, first identified by the New York State health department in mid-April as a sublineage that spreads even faster than BA.2, is now causing more than one-third of new COVID-19 cases in the country, according to CDC estimates. In New York and New Jersey, BA.2.12.1 is causing over 60% of new cases; it’s no coincidence that these states are also reporting some of the highest case and hospitalization rates in the country right now. New England, mid-Atlantic, South, and Midwest states are also seeing high proportions of BA.2.12.1. The CDC’s variant proportions estimates don’t yet include BA.4 and BA.5, but other reports suggest that these subvariants are already in the U.S. and starting to compete with our homegrown BA.2 lineages. Marc Johnson, a leading wastewater expert in Missouri, posted on Twitter yesterday that he’s seeing “a circus of Omicron sublineages” in his state, including BA.4 and BA.5. Also worth noting: a new U.S. study (shared as a preprint last week) found that, actually, Omicron is not inherently less severe than other variants. In comparing hospitalization and mortality risks after accounting for vaccination and medical risk factors, the researchers behind this study found little difference between the Omicron wave and prior periods. While this study also has yet to be peer-reviewed, it doesn’t bode well for future Omicron-driven surges.
In parts of the country with low vaccination rates, the variant may be responsible for up to 90% of sequenced cases, officials said. The rapidly spreading Delta variant now accounts for 83% of sequenced Covid-19 cases in the United States, the nation’s public health leaders said Tuesday, and in parts of the country with low vaccination rates, it may be responsible for up to 90%. Rochelle Walensky, the director of the Centers for Disease Control and Prevention, told a congressional hearing the new 83% estimate represents “a dramatic increase” from 50% of sequenced cases that were tallied the week of July 3. In some parts of the country that percentage is even higher, particularly in areas with low vaccination rates, said Anthony Fauci, head of the National Institute of Allergy and Infectious Diseases. As the variant has spread, Covid-19 deaths in the U.S. have risen, climbing by nearly 48% over the past week and now averaging 239 per day, she said. “We know the majority of deaths could be prevented by vaccination,” Walensky said. Vaccination has been uneven, with levels below half of eligible people in two-thirds of the country, Walensky said. She cited a five-month CDC study that found 99.5% of Covid-19 deaths are among people who are unvaccinated.
“The best way to prevent the spread of Covid-19 variants is to prevent the spread of disease. And vaccination is the most powerful tool we have,” she said. “We must continue to expand vaccine coverage by building trust and confidence in Covid-19 vaccines. And this is particularly important in communities of color, rural communities, and other population groups at risk.” Pressed to explain why the U.S. has not pursued booster shots as Israel has done with third Pfizer doses, Walensky and Fauci both pushed back. Walensky said the CDC is sharing data with Israel and the U.K. “where they’re several weeks ahead of us in the variant,” while watching more than 20 cohorts of vaccine recipients for any signs that their protection against Covid-19 might be waning. So far protection from recognizable disease continues to hit percentages in the low 90s, Fauci said. “If you see it fall below that into the 80s or even, unfortunately, I hope it never happens, into the 70s, then, you know, you reach the point where the durability needs a boost,” he said. “Those studies are ongoing right now.” Fauci blamed the variant’s high transmissibility for the surge in cases among unvaccinated people. First identified in India, Delta has swept through 90 countries around the world. But the three vaccines approved in the U.S. — mRNA vaccines from Moderna and Pfizer and the adenovirus-delivered vaccine from Johnson & Johnson — continue to be highly effective against Delta and other variants. “We have the tools to end this epidemic,” Fauci told the Senate Committee on Health, Education, Labor and Pensions. “It’s up to us to use those tools to the maximum.”
The United States hit a record high number of confirmed daily coronavirus cases Friday, recording more than 83,000 new cases, according to data compiled by Johns Hopkins University. The number surpasses the previous record of more than 77,000 cases in mid-July. The U.S. also recorded 943 deaths due to COVID-19 on Friday. More than 8 million people in the U.S. have been infected with the virus, and more than 223,000 people have died from the disease since the pandemic began, according to Johns Hopkins University. More than 42 million cases have been reported worldwide. One day earlier, 71,671 new coronavirus cases were reported in the U.S. on Thursday. Cases have been rising sharply in the U.S. since mid-September, with new outbreaks picking up in several states. Hospitalizations have also been on the rise.
The COVID Tracking Project reports 41,485 coronavirus patients were hospitalized as of Friday. The number is more than half of the highs recorded during the coronavirus surges in the spring and summer. Unlike past surges, where a few states drove up case numbers, the current high is being propelled by many states. Texas currently has the most recorded cases, followed by Illinois, Wisconsin and Florida. Despite the rise in cases, there has been some good news. Two peer-reviewed studies recently showed a drop in mortality among patients hospitalized with COVID-19, suggesting health care workers have gotten better at helping patients survive the disease. One study found that the mortality rate among hospitalized patients dropped from 25.6 percent to 7.6 percent. The mortality rate remains high compared with other diseases, and some continue to suffer complications long after recovering.
The new coronavirus spread across much of the interior of the United States by tagging along with people moving from state to state, but US coastal regions were seeded with SARS-CoV-2 imported from other countries — perhaps in 2019, according to models. Alessandro Vespignani at Northeastern University in Boston, Massachusetts, and his colleagues studied air traffic, commuting patterns and other data to understand how and when the coronavirus took hold in the United States (J. T. Davis et al. Preprint at medRxiv http://doi.org/d3mf; 2020). The team found that in several coastal states, international travel drove introduction of the virus. In California and New York, SARS-CoV-2 might have begun circulating as early as December 2019.
But in many non-coastal states, domestic travelers rather than international visitors were the source of the first wave of infections. Infections spread across the country from late January to early March but were largely undetected, the authors say. The findings have not yet been peer reviewed.
Preprint of original study available at medRxiv (July 7, 2020):
Since February 14 through March 16, a total of 4,226 COVID-19 cases had been reported in the United States, with reports increasing to 500 or more cases per day beginning March 14. 31% of cases, 45% of hospitalizations, 53% of ICU admissions, and 80% of deaths occurred among adults aged ≥65 years with the highest percentage of severe outcomes among persons aged ≥85 years. These findings are similar to data from China, which indicated >80% of deaths occurred among persons aged ≥60 years. These preliminary data also demonstrate that severe illness leading to hospitalization, including ICU admission and death, can occur in adults of any age with COVID-19. In contrast, persons aged ≤19 years appear to have milder COVID-19 illness, with almost no hospitalizations or deaths reported to date in the United States in this age group. Given the spread of COVID-19 in many U.S. communities, CDC continues to update current recommendations and develop new resources and guidance, including for adults aged ≥65 years as well as those involved in their care.
This report describes the current epidemiology of COVID-19 in the United States, using preliminary data. The findings in this report are subject to at least five limitations. First, data were missing for key variables of interest. Data on age and outcomes, including hospitalization, ICU admission, and death, were missing for 9%–53% of cases, which likely resulted in an underestimation of these outcomes. Second, further time for follow-up is needed to ascertain outcomes among active cases. Third, the initial approach to testing was to identify patients among those with travel histories or persons with more severe disease, and these data might overestimate the prevalence of severe disease. Fourth, data on other risk factors, including serious underlying health conditions that could increase risk for complications and severe illness, were unavailable at the time of this analysis. Finally, limited testing to date underscores the importance of ongoing surveillance of COVID-19 cases. Additional investigation will increase the understanding about persons who are at risk for severe illness and death from COVID-19 and inform clinical guidance and community-based mitigation measures
CDC Morbidity and Mortality Weekly Report (March 18, 2020): |