Your new post is loading...

|
Scooped by
Juan Lama
|
Scientists can now spot key differences in the blood of people who have long Covid symptoms— and those who don't. More than three years into the pandemic, the millions of people who have suffered from long Covid finally have scientific proof that their condition is real. Scientists have found clear differences in the blood of people with long Covid — a key first step in the development of a test to diagnose the illness. The findings, published Monday in the journal Nature, also offer clues into what could be causing the elusive condition that has perplexed doctors worldwide and left millions with ongoing fatigue, trouble with memory and other debilitating symptoms. The research is among the first to prove that "long Covid is, in fact, a biological illness," said David Putrino, principal investigator of the new study and a professor of rehabilitation and human performance at the Icahn School of Medicine at Mount Sinai in New York. Dr. Marc Sala, co-director of the Northwestern Medicine Comprehensive Covid-19 Center in Chicago, called the findings "important." He was not involved with the new research. "This will need to be investigated with more research, but at least it's something because, quite frankly, right now we don't have any blood tests" either to diagnose long Covid or help doctors understand why it's occurring, he said. Putrino and his colleagues compared blood samples of 268 people. Some had Covid but had fully recovered, some had never been infected, and the rest had ongoing symptoms of long Covid at least four months after their infection. Several differences in the blood of people with long Covid stood out from the other groups. The activity of immune system cells called T cells and B cells — which help fight off germs — was "irregular" in long Covid patients, Putrino said. One of the strongest findings, he said, was that long Covid patients tended to have significantly lower levels of a hormone called cortisol. A major function of the hormone is to make people feel alert and awake. Low cortisol could help explain why many people with long Covid experience profound fatigue, he said. "It was one of the findings that most definitively separated the folks with long Covid from the people without long Covid," Putrino said. The finding likely signals that the brain is having trouble regulating hormones. The research team plans to dig deeper into the role cortisol may play in long Covid in future studies. Meanwhile, doctors do not recommend simply boosting a person's cortisol levels in an attempt to "fix" the problem... Study published in Nature (Sept. 25, 2023): https://doi.org/10.1038/s41586-023-06651-y

|
Scooped by
Juan Lama
|
Low cortisol levels and herpes-virus reactivation are associated with prolonged COVID-19 symptoms, preliminary research suggests. Researchers looking for biological drivers and markers of long COVID have linked the syndrome to herpes viruses, as well as to reduced levels of a stress hormone1. The exploratory study drew both praise and criticism from scientists contacted by Nature. “A major weakness of this paper is the very small sample size,” says infectious-disease specialist Michael Sneller at the US National Institute of Allergy and Infectious Diseases (NIAID) in Bethesda, Maryland. “I would take with a huge grain of salt all these findings unless they are confirmed in larger studies.” But Danny Altmann, an immunologist at Imperial College London who was not involved in the study, says such reports are exactly what the long-COVID research community needs. “We’re really desperate to work out which drugs to test” for long COVID, he says. “The more studies we have like this, the more it enables us to race off and plan appropriate randomized, controlled trials.” The study, posted on the preprint server medRxiv, has not yet been peer reviewed. The disease that lingers Long COVID consists of a constellation of sometimes debilitating symptoms that last for months or years after a SARS-CoV-2 infection. It is common — affecting anywhere from 5% to 50% of people who contract COVID-19 — but researchers have few clues to its causes. The latest study, led by immunobiologist Akiko Iwasaki at Yale School of Medicine in New Haven, Connecticut, involved performing tests that generated thousands of data points for each of 215 participants in an attempt to reveal key immunological features that distinguish people with long COVID from healthy individuals. The study included 99 people with long COVID — those who reported persistent symptoms after SARS-CoV-2 infection — and 116 healthy participants who had either never had COVID-19 or had recovered after SARS-CoV-2 infection. Most strikingly, the study found that in the long-COVID group, levels of cortisol, a stress hormone that has a role in regulating inflammation, blood sugar levels and sleep cycles, were about 50% lower than in healthy participants. The authors also found hints that in people with long COVID, Epstein–Barr virus, which can cause mononucleosis, and varicella-zoster virus, which causes chickenpox and shingles, might recently have been ‘reactivated’. Both of these viruses are in the herpes family, persist indefinitely in the body after infection and can start to multiply again after a period of quiescence. People in the long-COVID group also had unusual levels of certain types of blood and immune cell, as well as dysfunctional immune cells, suggesting that their immune systems are working overtime. Iwasaki cautions that the results do not suggest that low cortisol levels or herpes viruses cause long COVID, but that their association with the syndrome warrants further study. The findings build on previous reports associating low cortisol levels and Epstein–Barr virus with long COVID, including a Cell paper2 published in March. With only 215 participants, the Iwasaki’s study is relatively small, and only a subset of the participants were included in some parts of the work. For example, in the analysis of cortisol levels, the researchers included all 99 people with long COVID, but only 40 of the 116 healthy people. “The small number of controls compared to the long-COVID group is problematic” because it makes the study less statistically robust, says Sneller, who is leading a separate study on the drivers of long COVID. Iwasaki says that samples were collected from the remaining healthy volunteers later and are being sent for analysis this week. Another limitation of the study is that Iwasaki’s team did not analyse participants’ samples for the presence of the Epstein–Barr and varicella-zoster viruses, instead measuring levels of antibodies against the viruses. Members of the long-COVID group had higher levels of these antibodies than did the healthy people, which suggests a more recent reactivation of the virus, Iwasaki says. However, the only way to determine definitively whether there is current reactivation is to test for viral DNA in the blood. Iwasaki’s team is now running such tests. Her group also plans to test participants’ cortisol levels throughout the day, because the stress hormone’s levels tend to fluctuate, and to examine how immune features vary at different time points after infection. “This is an exploratory, hypothesis-generating study, and clearly not the conclusion to what long COVID is, but it does begin to open doors,” says Iwasaki. Published in Nature (August 25, 2022): https://doi.org/10.1038/d41586-022-02296-5
|

|
Scooped by
Juan Lama
|
“Long COVID” in some may not be an entirely new entity, researchers say. COVID can cause reservoirs of some viruses you’ve previously battled to reactivate, potentially leading to symptoms of chronic fatigue syndrome—a condition that resembles long COVID, a recent study found. You had COVID a few months ago and recovered—but things still aren’t quite right. When you stand up, you feel dizzy, and your heart races. Even routine tasks leave you feeling spent. And what was once a good night’s sleep no longer feels refreshing. Long COVID, right? It may not be so simple. A mild or even an asymptomatic case of COVID can cause reservoirs of some viruses you’ve previously battled to reactivate, potentially leading to symptoms of chronic fatigue syndrome—a condition that resembles long COVID, according to a recent study published in the journal Frontiers in Immunology. Researchers found herpes viruses like Epstein-Barr, one of the drivers behind mono, circulating in unvaccinated patients who had experienced COVID. In patients with chronic fatigue syndrome, antibody responses were stronger, signaling an immune system struggling to fight off the lingering viruses. Such non-COVID pathogens have been named as likely culprits behind chronic fatigue syndrome, also known as myalgic encephalomyelitis. The nebulous condition with no definitive cause leads to symptoms like fatigue, brain fog, dizziness when moving, and unrefreshing sleep. The symptoms of many long COVID patients could be described as chronic fatigue syndrome, experts say. Researchers in the October study hypothesized that COVID sometimes leads to suppression of the immune system, allowing latent viruses reactivated by the stress of COVID to recirculate—viruses linked to symptoms that are common in Chronic Fatigue Syndrome and long COVID. Thus, “long COVID” in some may not be an entirely new entity, but another postviral illness—like ones seen in some patients after Ebola, the original SARS of 2003–2004, and other infections—that overlaps with chronic fatigue syndrome. As top U.S. infectious disease expert Dr. Anthony Fauci said in 2020, long COVID “very well might be a postviral syndrome associated with COVID-19.” ‘We’re still not doing that’ It’s possible that COVID is reactivating latent viruses in at least a portion of long COVID patients, causing chronic fatigue syndrome symptoms, Dr. Alba Miranda Azola, codirector of the long COVID clinic at Johns Hopkins University School of Medicine, told Fortune. But her clinic doesn’t check for the reactivation of viruses in long COVID patients. She doesn’t think the possibility of such viruses causing symptoms in patients is worth giving those patients antivirals or antibiotics, which can lead to undesirable side effects. “We don’t have enough evidence to support that treatment,” she said. Other physicians who have prescribed such treatments for long COVID patients, and those patients didn’t see much improvement, Azola added. She recently asked an infectious disease colleague if it was standard practice to test for, and treat, latent viruses in long COVID patients. “We’re still not doing that,” she recalled him saying. Dr. Nir Goldstein, a pulmonologist at National Jewish Health in Denver, who runs the hospital’s long COVID clinic, said it’s not yet clear what role latent viruses play in the long COVID. That’s because the nascent condition is such a complex and varied disorder. A consensus definition for long COVID hasn’t been universally agreed upon. Hundreds of possible symptoms have been identified, he points out—and no single explanation can account for them all. “There may be an association, but it’s very hard to know the causation,” Goldstein said. “It could be the other way around—it could be that long COVID causes reactivation, not that reactivation causes long COVID.” Dr. Panagis Galiasatos, an assistant professor at Johns Hopkins’ pulmonary and critical care division who treats long COVID patients, doesn’t routinely test his patients for latent viruses, given that most respond well to treatments that his clinic uses. “If a patient doesn’t respond to treatment, maybe we’ll test for other things,” he said. There is a strong possibility that COVID is weakening the immune systems of “a good deal of people,” Galiasatos added. “I do think the immunodeficiency—when it’s there, it’s transient—allows those viruses to reemerge,” he said. Scientists are still unsure if viruses like Epstein-Barr merely initiate chronic fatigue syndrome or keep symptoms going, the October study points out. Similarly, researchers are still unsure what, if any, role latent viruses—including, potentially, SARS-CoV-2 itself—play in the development of long COVID. Few options, for now With so little known about both long COVID and chronic fatigue syndrome, it doesn’t really matter which a patient has, experts say—at least not right now. While the symptoms of both can be treated, there’s no specific drug for either because the cause—or causes—remain up in the air. “It’s the main reason why I don’t even order the test,” Azola said of antibody tests for possible latent viruses in long COVID patients. “There’s no treatment targeting chronic fatigue syndrome. There certainly are treatments that can help with symptom management and improve quality of life, but they’re not curative.” Delineating the two conditions could matter in the future, Goldstein said, if researchers can prove that the conditions are caused by residual viruses and develop a way to eradicate them. Azola has several patients who were diagnosed with chronic fatigue syndrome before COVID, after Epstein-Barr virus or H1N1 flu infections. They caught COVID, and now their chronic fatigue symptoms are much worse, she says. “They remember the things that worked for them before, learning how to pace themselves, staying out of what I call the corona-coaster—when they’re feeling good, doing a lot, then crashing for days,” she said. “They’re able to identify with that and implement strategies that have worked for them in the past.” Galiasatos, from Johns Hopkins, hopes that the new year brings long COVID breakthroughs, including a deeper understanding of the condition and tailored treatments—potentially by the end of 2023. Stanford University is recruiting for a study based on a theory similar to the one in the October study—that long COVID is caused by a lingering reservoir of the SARS-CoV-2 virus, which causes COVID, after acute infection. It will attempt to determine if the antiviral drug Paxlovid alleviates long COVID symptoms by reducing or eliminating that viral reservoir. “We’re starting to move into the trial-treatment phase slowly,” Azola said. Study Cited Published in Frontiers in Immunology: https://doi.org/10.3389/fimmu.2022.949787

|
Scooped by
Juan Lama
|
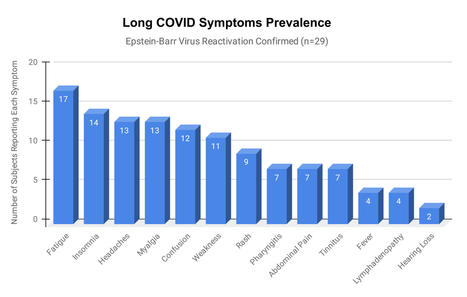
Epstein-Barr virus (EBV) reactivation resulting from the inflammatory response to coronavirus infection may be the cause of previously unexplained long COVID symptoms—such as fatigue, brain fog, and rashes—that occur in approximately 30% of patients after recovery from initial COVID-19 infection. The first evidence linking EBV reactivation to long COVID, as well as an analysis of long COVID prevalence, is outlined in a new long COVID study published in the journal Pathogens. "We ran EBV antibody tests on recovered COVID-19 patients, comparing EBV reactivation rates of those with long COVID symptoms to those without long COVID symptoms," said lead study author Jeffrey E. Gold of World Organization. "The majority of those with long COVID symptoms were positive for EBV reactivation, yet only 10% of controls indicated reactivation." The researchers began by surveying 185 randomly selected patients recovered from COVID-19 and found that 30.3% had long term symptoms consistent with long COVID after initial recovery from SARS-CoV-2 infection. This included several patients with initially asymptomatic COVID-19 cases who later went on to develop long COVID symptoms. The researchers then found, in a subset of 68 COVID-19 patients randomly selected from those surveyed, that 66.7% of long COVID subjects versus 10% of controls were positive for EBV reactivation based on positive EBV early antigen-diffuse (EA-D) IgG or EBV viral capsid antigen (VCA) IgM titers. The difference was significant (p < 0.001, Fisher's exact test). "We found similar rates of EBV reactivation in those who had long COVID symptoms for months, as in those with long COVID symptoms that began just weeks after testing positive for COVID-19," said coauthor David J. Hurley, Ph.D., a professor and molecular microbiologist at the University of Georgia. "This indicated to us that EBV reactivation likely occurs simultaneously or soon after COVID-19 infection." The relationship between SARS-CoV-2 and EBV reactivation described in this study opens up new possibilities for long COVID diagnosis and treatment. The researchers indicated that it may be prudent to test patients newly positive for COVID-19 for evidence of EBV reactivation indicated by positive EBV EA-D IgG, EBV VCA IgM, or serum EBV DNA tests. If patients show signs of EBV reactivation, they can be treated early to reduce the intensity and duration of EBV replication, which may help inhibit the development of long COVID. "As evidence mounts supporting a role for EBV reactivation in the clinical manifestation of acute COVID-19, this study further implicates EBV in the development of long COVID," said Lawrence S. Young, Ph.D., a virologist at the University of Warwick, and Editor-in-Chief of Pathogens. "If a direct role for EBV reactivation in long COVID is supported by further studies, this would provide opportunities to improve the rational diagnosis of this condition and to consider the therapeutic value of anti-herpesvirus agents such as ganciclovir." Original findings published in Pathogens (June 10, 2021): https://doi.org/10.3390/pathogens10060763
|



 Your new post is loading...
Your new post is loading...