In this journal E. Orviz and colleagues recently described the clinical presentation of the first monkeypox patients in Spain, highlighting the frequent co-presence of sexually transmitted infections (STI). To date, no reports of co-infection with monkeypox virus and SARS-CoV-2 have been published. Therefore, in this study we present the clinical features and diagnostic procedure of the first documented case of co-infection with monkeypox virus, SARS-CoV-2 and HIV-1. Since January 2022, more than 16,000 people in over 74 countries have been affected by monkeypox, prompting the World Health Organization to declare this outbreak a public health emergency of international concern. Human-to-human transmission occurs through close contact with infectious material from skin lesions, fomites, seminal fluids and oropharyngeal secretions. The majority of cases were registered in gay or bisexual men often suffering from other STI. At the same time, SARS-CoV-2 is still a major cause of morbidity and mortality globally. COVID-19 shares with monkeypox both the transmission by air droplets and the symptoms of fever, lymphadenopathy, headache, sore throat and fatigue. As these pathogens continue to spread, individuals can be simultaneously infected with monkeypox virus, SARS-CoV-2 and STI, making it difficult for physicians to perform the correct diagnosis, also considering that not all patients with monkeypox develop skin lesions.
Our patient, an Italian 36-year-old male spent 5 days in Spain from 16 to 20 June 2022 (Figure 1). Nine days after, he developed fever (up to 39°C), accompanied by sore throat, fatigue, headache and right inguinal lymphadenomegaly. On 2 July he resulted positive for SARS-CoV-2. On the afternoon of the same day a rash started to develop on his left arm. The following day small, painful vesicles surrounded by an erythematous halo appeared on the torso, lower limbs, face and glutes. On 5 July, due to a progressive and uninterrupted spread of vesicles that began to evolve into umbilicated pustules, he went to the emergency department of the Policlinico “G. Rodolico - San Marco” University Hospital in Catania, Italy, and was subsequently transferred to the Infectious Diseases unit. On admission, the patient reported being treated for syphilis in 2019. In September 2021, he performed an HIV test with a negative result. He suffered from bipolar disorder, for which he regularly took carbamazepine 200 mg daily. He was vaccinated for SARS-CoV-2 with two doses of Pfizer's BNT162b2 mRNA vaccine (the last in December 2021) and had already contracted COVID-19 in January 2022. He also reported of having condomless intercourse with men during his stay in Spain. Fever (37.5°C), pharyngodynia, fatigue, headache was still present.
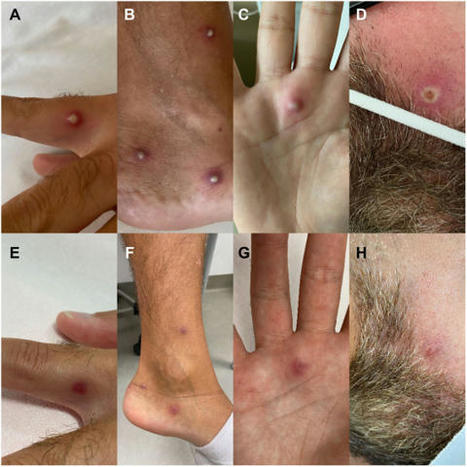
On physical examination his body was dotted, including the palm of the right hand and the perianal region, with skin lesions in various stages of progression, ranging from small vesicles (Figure 1, Panel A) to reddened haloed pustules (Figure 1, Panel B and Panel C) and umbilicated plaques (Figure 1, Panel D). The oral mucosa was normal, except for bilateral tonsillar hypertrophy. A modest hepatosplenomegaly and an enlarged (2 cm), hypomobile and painful lymph node in the right inguinal region were found. Laboratory test showed elevated C-reactive protein (69 mg/L, normal values 0.0 - 5.0 mg/L), fibrinogen (713 mg/dL, normal values 170 - 400 mg/dL) and prothrombin time (1.21, normal values 0.8 - 1.2). Chest X-ray revealed a parenchymal hypodiaphany in the right parailary region...
Published in Journal of Infection (August 19, 2022):



 Your new post is loading...
Your new post is loading...