In vivo CRISPR genome-wide screening pinpoints the transcriptional modulator CITED2 as a pivotal driver in the progression of prostate cancer to bone metastasis.
Get Started for FREE
Sign up with Facebook Sign up with X
I don't have a Facebook or a X account

 Your new post is loading... Your new post is loading...
 Your new post is loading... Your new post is loading...
A new light-inducible RNA base editing tool, padCas13, combines the specificity of CRISPR-Cas13 with the control of light activation and allows for precise, reversible RNA targeting and degradation in mammalian cells, both in vitro and in vivo.
BigField GEG Tech's insight:
The padCas13 editor can efficiently edit A-to-I and C-to-U RNA bases, targeting disease-relevant transcripts. Photoactivatable base editing represents a significant advance in CRISPR technology, as it enables fine-tuning of gene expression and post-translational modifications without permanent alterations to the genome. This method is particularly relevant for diseases in which transient modulation of gene expression may have therapeutic benefits. A crucial element of padCas13 is the Magnet system, which comprises a positively and negatively charged Magnet protein. These proteins are designed to heterodimerize rapidly in response to light, thereby activating the Cas13 nuclease.
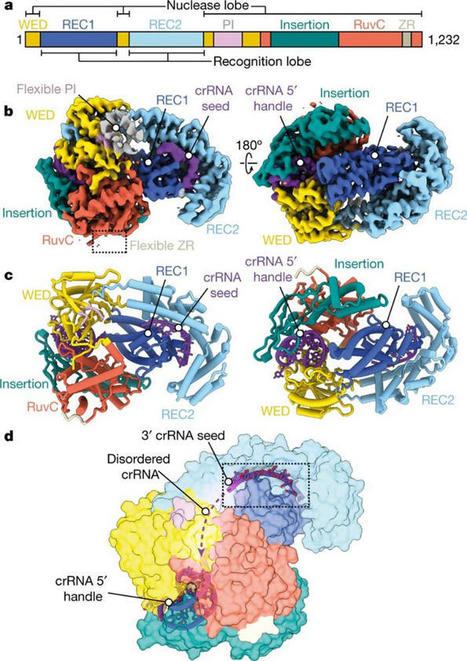
The recent publication in Science by Mogila, Tamulaitiene et al. represents a continuation of the successful scientific research conducted by Gintautas Tamulaitis' group.
BigField GEG Tech's insight:
In a recent study published in Science, researchers characterized a new family of effector proteins, named Cami1, using bioinformatics, biochemical and structural studies. They showed that when a virus attacks a bacterium, CRISPR-Cas10 signaling molecules activate Cami1, a ribosome-dependent ribonuclease. Activated Cami1 cleaves mRNAs involved in protein synthesis, inhibiting cell growth. This saves resources and prevents the production of viral proteins. Cami1's interaction with a specialized ribosomal structure, called a ribosomal stalk, is necessary for its entry into the protein synthesis center. Interestingly, the same capture mechanism to bind the ribosome is used by plant antiviral proteins that also inactivate ribosomes. This discovery has unveiled an additional layer of the CRISPR-Cas antiviral defense system and demonstrated a common antiviral strategy shared between eukaryotes and bacteria. Knowledge of our characterized Cami1 proteins will contribute to the development of new molecular tools in biotechnology and therapy
The gene editing technique CRISPR/Cas9 has allowed researchers to make precise and impactful changes to an organism's DNA to fix mutations that cause genetic disease.
BigField GEG Tech's insight:
CRISPR/Cas9 method can lead to unintended DNA mutations that can have negative effects. Recently, Japanese researchers have developed a new gene-editing technique that is as effective as CRISPR/Cas9, yet significantly reduces these unintended mutations. In a new study published in Nature Communications , researchers led by Osaka University have introduced a new technique called NICER, based on the creation of several small cuts in single DNA strands by an enzyme Cas 9 nickase. For their first experiments, the research team used human lymphoblastic cells with a known heterozygous mutation in a gene called TK1. When these cells were treated with nickase to induce a single cut in the TK1 region, TK1 activity was recovered at a low rate. However, when nickase induced multiple cuts in this region on both homologous chromosomes, the efficiency of gene correction was increased approximately seventeen-fold via activation of a cellular repair mechanism. Because the NICER method does not involve DNA double-strand breaks or the use of exogenous DNA, this technique appears to be a safe alternative to conventional CRISPR/Cas9 methods.
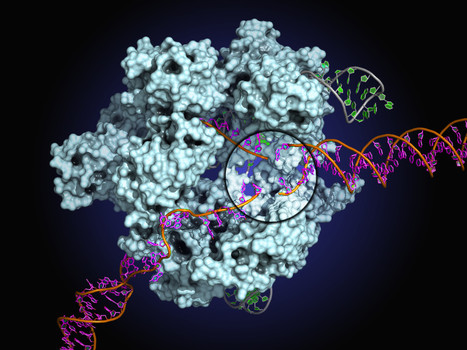
Scientists at Leipzig University, in collaboration with colleagues at Vilnius University in Lithuania, have developed a new method to measure the smallest twists and torques of molecules within milliseconds.
BigField GEG Tech's insight:
With the help of an embedded RNA, CRISPR complexes recognize a short DNA sequence. To better understand this process, researchers took advantage of the fact that the DNA double helix of the target sequence is unwound during recognition to allow base pairing with the RNA. Using a technique known as DNA origami, the researchers constructed a 75 nm-long DNA rotor arm with a gold nanoparticle attached to its end. In the experiment, the unwinding of the 2 nm thick, 10 nm long DNA sequence was transferred to the rotation of the gold nanoparticle along a 160 nm diameter circle: this movement could be amplified and tracked using a special microscope setup. With this new method, the researchers were able to observe sequence recognition by the CRISPR complex almost base pair by base pair. Surprisingly, base pairing with RNA is not energetically advantageous, meaning that the complex is only unstably bound during sequence recognition. Only when the entire sequence is recognized does stable binding occur, and the DNA is then destroyed. The sometimes erroneous results are due to its stochastic nature, i.e. random molecular movements.
Induced pluripotent stem (iPS) cells have a great impact on biology and medicine, and they are expected to improve regenerative medicine.
BigField GEG Tech's insight:
Fabry disease is caused by a genetic deficiency of α-galactosidase A (GLA), leading to the accumulation of its substrates such as globotriaosylceramide and globotriaosylsphingosine. Researchers have therefore developed a modified enzyme, modified α-N-acetylgalactosaminidase (mNAGA), to cure Fabry disease by changing the substrate specificity of NAGA to that of GLA. In this study, researchers tested whether genome-editing transplantation of mNAGA-secreting induced pluripotent stem cells (iPS) cells could deliver GLA activity in vivo. They therefore generated mNAGA-secreting iPS cells by TALEN-mediated knock-in at the AAVS1 site, a refuge locus. Furthermore, to exclude possible immunogenic reactions caused by endogenous GLA from iPS cells in patients, they disrupted the GLA gene by CRISPR-Cas9. When cardiomyocytes and fibroblasts from the Fabry model without GLA activity were co-cultured with mNAGA-secreting iPS cells, GLA activity was restored by mNAGA-expressing cells in vitro. Next, they transplanted the mNAGA-secreting iPS cells into the testes of mouse models of Fabry disease. After 7 or 8 weeks, GLA activity in the liver was significantly improved, although no recovery of activity was observed in the heart, kidneys or blood plasma.
BigField GEG Tech's insight:
Overall survival for patients with melanoma that has spread to the brain is only four to six months. Researchers have therefore investigated a new therapeutic approach to more effectively target melanoma in the brain. The therapy devised by the scientists uses a "twin stem cell model" designed to maximize an attack on cancer cells that have spread to a part of the brain known as the leptomeninges. A stem cell releases a cancer-killing virus (oncolytic). Using stem cells to deliver the virus amplifies the amount of virus that can be released, and ensures that the virus will not be degraded by circulating antibodies before it is released on cancer cells. However, the oncolytic virus also destroys the cells that release it, making it an unsustainable therapeutic option. Therefore, scientists have used CRISPR/Cas9 gene editing to create a second stem cell that cannot be targeted by the oncolytic virus and instead releases proteins (immunomodulators) that boost the immune system to help fight cancer. Twin stem cells can be delivered by intrathecal injection. Unlike other immunotherapies that have appeared in recent years, it does not need to be administered repeatedly. The researchers point out that this approach can be used in other cancers with metastases.
CRISPR-Cas9 is widely used to edit the genome by studying genes of interest and modifying disease-associated genes.
BigField GEG Tech's insight:
One of the drawbacks of genome editing is that there are growing concerns about mutations and off-target effects. Researchers then hypothesized that current editing protocols that use Cas9 cause excessive DNA cleavage, resulting in some of the mutations. To test this hypothesis, the researchers built a system called "AIMS" in mouse cells, which assessed Cas9 activity separately for each chromosome. Their results showed that the commonly used method was associated with very high editing activity. They determined that this high activity caused some of the undesirable side effects, so they looked for gRNA editing methods that could suppress it. They found that an additional cytosine extension at the 5' end of the gRNA was effective as a "safeguard" against overactivity and controlled DNA cleavage. As a result of this study, the first mathematical model of the correlation between various genome editing patterns and Cas9 activity was created that can maximize the desired editing efficiency by developing activity-regulating gRNAs with appropriate Cas9 activity.
Researchers from Utah State University and Germany’s Helmholtz Institute for RNA-based Infection Research demonstrate that upon recognition of an RNA target, Cas12a2 cleaves all the other nucleic acids present, destroying the bacterial cell and preventing bacteriophage from replicating.
BigField GEG Tech's insight:
Despite its phylogenetic placement with DNA-targeting nucleases, Cas12a2 targets and cleaves RNA. When researchers put Cas12a2 in test tubes with pure DNA and a guide, nothing happened, because its target was not present and it remained inactive. However, sometimes a small amount of activating RNA was present, contaminating the sample. When the RNA was present and Cas12a2 recognized its target, it destroyed all nucleic acids in the tube. Unlike the CRISPR-Cas9 system, when Cas12a2 finds its target, the infected cell(s) die. This mechanism is known as abortive infection. One of the obvious applications of Cas12a2 is in CRISPR diagnostics. It can easily be reprogrammed to detect certain targets, such as RNA viruses, with high specificity. The researchers have already demonstrated the feasibility of this approach in their recent work. Cas12a2 could also be programmed to kill specific cell types, such as tumor cells, for therapeutic purposes.
A new tool to predict the chances of successfully inserting a gene-edited sequence of DNA into the genome of a cell, using a technique known as prime editing, has been developed by researchers at the Wellcome Sanger Institute.
BigField GEG Tech's insight:
An evolution of the CRISPR-Cas9 gene editing technology, master editing has enormous potential to treat genetic diseases in humans. However, to date, the factors determining successful editing are not well understood. A new tool to predict the chances of successfully inserting a gene-edited DNA sequence into the genome of a cell has been developed by researchers. The study, published in Nature Biotechnology, evaluated thousands of different DNA sequences inserted into the genome using master editors. This data was then used to train a machine learning algorithm to help researchers design the best solution for a given genetic defect, promising to speed up efforts to introduce master editing into the clinic. Sequence length proved to be a key factor, as was the type of DNA repair mechanism involved. The next steps for the team will be to create models for all known human genetic diseases to better understand if and how they can be corrected using master editing.
Huntington’s disease (HD) is a fatal, dominantly inherited neurodegenerative disorder caused by CAG trinucleotide expansion in exon 1 of the huntingtin (HTT) gene. Since the reduction of pathogenic mutant HTT messenger RNA is therapeutic, we developed a mutant allele-sensitive CAGEX RNA-targeting CRISPR–Cas13d system (Cas13d–CAGEX) that eliminates toxic CAGEX RNA in fibroblasts derived from patients with HD and induced pluripotent stem cell-derived neurons. We show that intrastriatal delivery of Cas13d–CAGEX via an adeno-associated viral vector selectively reduces mutant HTT mRNA and protein levels in the striatum of heterozygous zQ175 mice, a model of HD. This also led to improved motor coordination, attenuated striatal atrophy and reduction of mutant HTT protein aggregates. These phenotypic improvements lasted for at least eight months without adverse effects and with minimal off-target transcriptomic effects. Taken together, we demonstrate proof of principle of an RNA-targeting CRISPR–Cas13d system as a therapeutic approach for HD, a strategy with implications for the treatment of other dominantly inherited disorders. Leveraging RNA-targeting CRISPR–Cas13d technology, Morelli et al. engineered a novel therapeutic strategy that safely and effectively eliminates toxic expanded huntingtin RNA in multiple models of Huntington’s disease.
BigField GEG Tech's insight:
Huntington's disease (HD) is a neurological disorder that causes progressive loss of movement, coordination and cognitive function. It is caused by a mutation in a single gene called huntingtin or HTT. In a new study, published Dec. 12, 2022, in Nature Neuroscience, researchers describe the use of CRISPR/Cas13d RNA-targeting technology to develop a new therapeutic strategy that specifically removes the toxic RNA that causes HD. They used viral vehicles to deliver the therapy to neuronal cultures, which were developed from stem cells derived from patients with HD, and found that the approach not only targeted and destroyed mutant RNA molecules, but also eliminated the accumulation of toxic proteins. They also demonstrated that the expression of other human genes was generally not disrupted by the therapy.
Last week, PACT Pharma shared results from the first clinical trial using CRISPR to direct patients’ immune cells to treat solid tumours. The findings, which were published in an unedited manuscript in Nature, provide early proof-of-concept that patient immune cells can be reprogrammed to attack their own cancer. The results were als
BigField GEG Tech's insight:
In most cases, the number of naturally occurring cancer-targeting T cells will be far too low to trigger an immune response capable of eradicating a patient's tumor(s). PACT Pharma is a privately held biopharmaceutical company developing personalized, neo-antigen-specific T-cell receptor (TCR)-T therapies to treat a range of solid tumors. Patient T cells are isolated and CRISPR-modified by electroporation with Cas9 protein, guide RNAs to knock out endogenous TCR genes (TCRα ( TRAC) and TCRβ ( TRBC)) and an HR template plasmid encoding the transgenic neoTCR. The results of a phase 1 clinical trial that were published in Nature. The researchers report that CRISPR-modified T cells were preferentially directed to the tumor and could be recovered from post-infusion biopsies in all patients for whom biopsies were available. They also note that CRISPR-edited T cells frequently accounted for the top 2-20% of immune cells in the tumor, and a reduction in tumor size was observed in some lesions in a single lung cancer patient.
Pierre-Luc Jellimann 's curator insight,
December 1, 2022 3:01 AM
Nouvelle article montrant l'efficaicté de CRISPR dans le traitement des tumeurs solides (first clinical trial using CRISPR to direct patients’ immune cells to treat solid tumours)
Researchers at Great Ormond Street Hospital for Children (GOSH) and UCL Great Ormond Street Institute of Child Health (UCL GOS ICH) have used CRISPR/Cas9 technology to engineer donor T cells to try to treat seriously ill children with resistant leukaemia, who had otherwise exhausted all available therapies.
BigField GEG Tech's insight:
Researchers have used CRISPR/Cas9 technology to engineer donor T cells to treat critically ill children with resistant leukemia who had otherwise exhausted all available therapies. The Phase I trial, published in Science Translational Medicine , is the first use of CRISPR-edited "universal" cells in humans and represents a significant advance in the use of genetically engineered cells for cancer treatment. In the trial, the research team constructed and applied a new generation of genome-edited "universal" T cells, which builds on previous work that used older, less precise technology. The T cells were modified using CRISPR. In addition, the piece of genetic code allows the T cells to express a CAR receptor that can recognize a marker on the surface of cancerous B cells and then destroy them. The T cells were then genetically modified with CRISPR so that they could be used "off the shelf" without the need for a donor match. In specialist clean rooms, researchers manufactured their banks of donor CAR T-cells using a single disabled virus to transfer both the CAR and a CRISPR guidance system, and then applied cutting-edge mRNA technology to activate the gene editing steps.
Pierre-Luc Jellimann 's curator insight,
November 17, 2022 3:03 AM
Researchers have used CRISPR/Cas9 technology to engineer donor T cells to treat critically ill children with resistant leukemia who had otherwise exhausted all available therapies. The Phase I trial, published in Science Translational Medicine , is the first use of CRISPR-edited "universal" cells in humans and represents a significant advance in the use of genetically engineered cells for cancer treatment. In the trial, the research team constructed and applied a new generation of genome-edited "universal" T cells, which builds on previous work that used older, less precise technology. The T cells were modified using CRISPR. In addition, the piece of genetic code allows the T cells to express a CAR receptor that can recognize a marker on the surface of cancerous B cells and then destroy them. The T cells were then genetically modified with CRISPR so that they could be used "off the shelf" without the need for a donor match. In specialist clean rooms, researchers manufactured their banks of donor CAR T-cells using a single disabled virus to transfer both the CAR and a CRISPR guidance system, and then applied cutting-edge mRNA technology to activate the gene editing steps. 
Singh's curator insight,
November 17, 2022 5:07 AM
Une thérapie génique et universelle. La technologie CRISPR/Cas9 est un espoir dans la thérapie de la leucémie résistante. Une attention toute particulière doit toutefois se porter sur l'insertion génétique qui doit être finement régulée afin d'éviter les effets délétères. 
Gilbert C FAURE's comment,
November 17, 2022 6:23 AM
allez voir sur https://www.scoop.it/topic/immunology-and-biotherapies quelques surprises déjà New study finds that CRISPR/Cas9 leads to unexpected genomic changes
|
Over the past two decades, the immune system has attracted increasing attention for its role in fighting cancer.
BigField GEG Tech's insight:
CRISPR-based gene editing has become a mainstay of biological discovery, providing relatively rapid insight into the function of individual genes and targets for new therapies. However, the main challenge is that it is difficult to edit immune cells without changing their biology, hampering the ability to study immune cell behavior in all its complexity in a living organism. In an earlier study, researchers used CHimeric IMmune Editing (CHIME) to knock out a gene called Ptpn2, which has shown promise for cancer immunotherapy. The recent study published in Nature Immunology explores methods to increase the precision and versatility of CHIME, including simultaneous deletion of multiple genes and targeted application in specific cell types, also using CRISPR to disrupt genes in the edited cells once they were already back inside the animal. This research has successfully demonstrated the feasibility of various innovative approaches to genetic manipulation, offering new avenues for the study of immune gene function.
Utilizing CRISPR screening, the deubiquitinase ATXN3 has been identified as a key regulator of PD-L1 transcription in tumor cells, a critical factor in tumor immune evasion.
BigField GEG Tech's insight:
Using CRISPR screening, the deubiquitinase ATXN3 was identified as a key regulator of PD-L1 transcription in tumor cells, a critical factor in tumor immune evasion. In this study, researchers transfected a targeted library of all 96 members of the mammalian deubiquitinase family into melanoma cells, then sorted the cells according to low and high PD-L1 expression to identify the regulators. ATXN3 was found to positively influence PD-L1 transcription, helping tumor cells to evade the immune system. This new insight represents a promising target for improving the efficacy of antitumor immunotherapy by blocking checkpoints, potentially transforming cancer treatment strategies. The study also highlights the broader role of ATXN3 in regulating tumor microenvironmental responses to hypoxia and inflammation, opening up new avenues for cancer research and treatment.
RAG2-SCID is a primary immunodeficiency caused by mutations in Recombination-activating gene 2 (RAG2), a gene intimately involved in the process of lymphocyte maturation and function. ex-vivo manipulation of a patient’s own hematopoietic stem and progenitor cells (HSPCs) using CRISPR-Cas9/rAAV6 gene editing could provide a therapeutic alternative to the only current treatment, allogeneic hematopoietic stem cell transplantation (HSCT). Here we show an innovative RAG2 correction strategy that replaces the entire endogenous coding sequence (CDS) for the purpose of preserving the critical endogenous spatiotemporal gene regulation and locus architecture. Expression of the corrective transgene leads to successful development into CD3+TCRαβ+ and CD3+TCRγδ+ T cells and promotes the establishment of highly diverse TRB and TRG repertoires in an in-vitro T-cell differentiation platform. Thus, our proof-of-concept study holds promise for safer gene therapy techniques of tightly regulated genes. RAG2-SCID is a primary immunodeficiency caused by mutations in Recombination-activating gene 2 (RAG2). Here the authors report a RAG2 correction strategy that replaces the entire endogenous coding sequence (CDS) to maintain the endogenous spatiotemporal gene regulation and locus architecture.
BigField GEG Tech's insight:
Severe combined immunodeficiency represents rare monogenic disorders with defects in humoral and cellular immunity. RAG genes code for proteins that initiate lymphoid-specific V(D)J recombination, essential for T and B lymphocyte maturation. As a result, individuals carrying pathogenic RAG variants are either completely devoid of, or possess far fewer, B and T cells. In a recent study, researchers described a CRISPR-Cas9-based genome-editing approach to replace the entire respective RAG2 coding sequences (CDS) with a corrective transgene in a 34-positive (CD34+) hematopoietic stem and progenitor cell (HSPC) differentiation cluster. Two recombinant adeno-associated virus serotype 6 (rAAV6) vectors were synthesized to integrate a green fluorescent protein expression cassette and a bovine growth hormone polyA sequence into CD34+ HSPCs after delivery of a single modified RAG2 guide RNA or the Cas9 ribonucleoprotein complex. The researchers' strategy completely replaced RAG2 CDS to treat autosomal recessive immunity disorders. The method induced expression of RAG2 coding DNA without exceeding endogenous RAG2 expression levels. Correction donors promoted the successful recombination and differentiation of V(D)J into CD3 + TCRγδ + and CD3 + TCRαβ + T cells.
Rochester Institute of Technology researchers are improving non-invasive treatment options for degenerative disc disease, an ailment that impacts 3 million adults yearly in the U.S., according to the Mayo Clinic.
BigField GEG Tech's insight:
Researchers are improving non-invasive treatment options for degenerative disc disease, a condition that affects 3 million adults each year in the U.S. Stem cell therapy has been a viable field in regenerative technologies for many pathologies for several years. However, the degenerated intervertebral disc provides a hostile environment that is detrimental to stem cell survival, resulting in limited clinical success of stem cell therapy for the disc. Previous research has shown that stem cell-derived electrical vehicles contain many therapeutically beneficial proteins, lipids and nucleic acids and carry much of the regenerative potential of stem cells. However, by using CRISPR in mesenchymal stem cells, researchers have added to the growing field of regenerative medicine the process of producing cell-based therapies to alleviate pain and lack of mobility. In their study, the researchers target TSG6, an essential stem cell marker known to be linked to the regenerative and anti-inflammatory properties of these stem cells. Their hypothesis is that if they CRISPR-activate TSG6 in stem cells, they will not only increase TSG6 protein levels in the extracellular vesicle cargo, but potentially amplify the stem cells' anti-inflammatory and regenerative properties.
Vaccine boosting modifies CAR T cell metabolism and promotes crosstalk between CAR
BigField GEG Tech's insight:
Engineering T cells to destroy cancer cells has proved effective in treating certain types of cancer. However, it has not worked as well for solid tumors. One of the reasons for this lack of success is that T cells only target a single antigen. If some of the tumor cells don't express this antigen, they can evade T cell attack. In 2019, researchers found a way to overcome this obstacle, using a vaccine that enhances CAR-T cell efficacy. In a recent study, researchers wanted to investigate how this additional T-cell response is activated. The researchers discovered that in these vaccinated mice, metabolic changes occur in CAR-T cells that increase their production of interferon gamma, a cytokine that helps stimulate a strong immune response. This helps T cells overcome the tumor's immunosuppressive environment, which normally shuts down all T cells in the vicinity. As CAR-T cells killed tumor cells expressing the target antigen, host T cells encountered other antigens from these tumor cells, stimulating these host T cells to target these antigens and help destroy the tumor cells. Without this host T-cell response, the researchers found that tumors would regrow even if CAR-T cells destroyed most of them.
Molecular routes to metastatic dissemination are critical determinants of aggressive cancers. Through in vivo CRISPR–Cas9 genome editing, we generated somatic mosaic genetically engineered models that faithfully recapitulate metastatic renal tumors. Disruption of 9p21 locus is an evolutionary driver to systemic disease through the rapid acquisition of complex karyotypes in cancer cells. Cross-species analysis revealed that recurrent patterns of copy number variations, including 21q loss and dysregulation of the interferon pathway, are major drivers of metastatic potential. In vitro and in vivo genomic engineering, leveraging loss-of-function studies, along with a model of partial trisomy of chromosome 21q, demonstrated a dosage-dependent effect of the interferon receptor genes cluster as an adaptive mechanism to deleterious chromosomal instability in metastatic progression. This work provides critical knowledge on drivers of renal cell carcinoma progression and defines the primary role of interferon signaling in constraining the propagation of aneuploid clones in cancer evolution. Using genetically engineered models, Genovese and colleagues study patterns of convergent evolution in renal cancer, and pinpoint dysregulation of interferon signaling as a means of adaptation to chromosomal instability in metastatic progression.
BigField GEG Tech's insight:
One of the hallmarks of renal cell carcinoma (RCC) is chromosomal instability, which is associated with resistance to many types of therapy and a poor prognosis. It is not known whether specific types of chromosomal abnormalities are involved in metastasis and how tumors are able to tolerate them. Researchers have used CRISPR/Cas9-based genome editing to generate models of aggressive renal cell carcinoma (RCC), lacking common tumor suppressor genes. Using genome sequencing and single-cell RNA sequencing to examine these models in more detail, the researchers uncovered the molecular drivers of RCC and gained a new understanding of the evolution of chromosomal instability. IFNR gene clusters are normally involved in the immune response. After analyzing various datasets from mice and humans, the researchers discovered an inverse correlation between the loss of these IFNR genes and aneuploidy, a condition characterized by an abnormal number of chromosomes. This study suggests that tumors adapt to high levels of chromosomal instability by disrupting the IFNR pathway, and that this is likely to be a major biomarker of metastatic potential. In future, the researchers plan to test drug combinations in these newly generated models to determine how tumors adapt to various therapies.
The most common form of genetic heart disease is hypertrophic cardiomyopathy (HCM), which is caused by variants in cardiac sarcomeric genes and leads to abnormal heart muscle thickening. Complications of HCM include heart failure, arrhythmia and sudden cardiac death. The dominant-negative c.1208G>A (p.R403Q) pathogenic variant (PV) in β-myosin (MYH7) is a common and well-studied PV that leads to increased cardiac contractility and HCM onset. In this study we identify an adenine base editor and single-guide RNA system that can efficiently correct this human PV with minimal bystander editing and off-target editing at selected sites. We show that delivery of base editing components rescues pathological manifestations of HCM in induced pluripotent stem cell cardiomyocytes derived from patients with HCM and in a humanized mouse model of HCM. Our findings demonstrate the potential of base editing to treat inherited cardiac diseases and prompt the further development of adenine base editor-based therapies to correct monogenic variants causing cardiac disease. Adenine base editing successfully corrected a MYH7 pathogenic variant that causes hypertrophic cardiomyopathy in human cardiomyocytes and a mouse model of the disease, highlighting the potential of the approach to correct monogenic variants causing cardiac disease.
BigField GEG Tech's insight:
The thickening of the heart muscle associated with hypertrophic cardiomyopathy leads to arrhythmia, heart failure and sudden cardiac death. The disease often goes undiagnosed, and heart transplantation is the only known treatment. Researchers have been working on a therapy using base editing to correct one of the mutations causing HCM. In this latest study, their target was a mutation in the myosin heavy chain 7 (MYH7) gene. MYH7 encodes β-myosin heavy chain, a motor ATPase that incorporates into heart muscle filaments and affects their contractions. Moreover, the pathogenic G-to-A mutation in the MYH7 gene studied is responsible for a severe, early-onset form of Crohn's disease. The team used the CRISPR-Cas 9 system to correct the MYH7 mutation in induced pluripotent stem cells derived from MHC patients, achieving extremely high editing efficiencies of up to 99%, with little or no off-target. The next step will be to obtain more data in a large animal model and make this potential therapy as safe as possible.
The expanding applications of nonviral genomic medicines in the lung remain restricted by delivery challenges. Here, leveraging a high-throughput platform, we synthesize and screen a combinatorial library of biodegradable ionizable lipids to build inhalable delivery vehicles for messenger RNA and CRISPR–Cas9 gene editors. Lead lipid nanoparticles are amenable for repeated intratracheal dosing and could achieve efficient gene editing in lung epithelium, providing avenues for gene therapy of congenital lung diseases. A high-throughput screen improves lipid nanoparticle delivery of gene editors in the lung.
BigField GEG Tech's insight:
Researchers are developing lipid nanoparticles that may target the lungs. The particles are made of molecules that contain two parts: a positively charged head group and a long lipid tail. The positive charge of the head group helps the particles interact with negatively charged mRNA, and also helps the mRNA escape from cellular structures that engulf the particles once they enter the cells. In tests on mice, the researchers showed that they could use the particles to deliver mRNA encoding CRISPR/Cas9 components designed to turn off a genetically encoded stop signal in the animals' lung cells. When this stop signal is removed, a gene for a fluorescent protein lights up. Measuring this fluorescent signal allows researchers to determine what percentage of cells have successfully expressed the mRNA. After one dose of mRNA, about 40% of lung epithelial cells were transfected, the researchers found. Two doses brought the level to more than 50% and three doses to 60%. The most important targets for treating lung disease are two types of epithelial cells called club cells and hair cells, and each was transfected at about 15%. These particles could offer an inhalable treatment for cystic fibrosis and other lung diseases.
The genetic mutation underlying a severe immune system deficiency can be corrected
BigField GEG Tech's insight:
The rare and fatal genetic disease CD3 delta severe combined immunodeficiency, also known as CD3 delta SCID, is caused by a mutation in the CD3D gene, which prevents the production of the CD3 delta protein needed for normal T cell development from blood stem cells. Currently, bone marrow transplantation is the only treatment available, but the procedure carries significant risks. In a study published in Cell, researchers showed that a new genome editing technique called base editing can correct the mutation that causes CD3 delta SCID in blood stem cells and restore their ability to produce T cells. The basic editor corrected an average of nearly 71 percent of the patient's stem cells in three experiments. The researchers then tested whether the corrected cells could give rise to T cells. When the corrected blood stem cells were introduced into artificial thymic organoids, they produced fully functional and mature T cells. The corrected cells remained four months after transplantation, indicating that the basic editing had corrected the mutation in the true self-renewing blood stem cells. The results suggest that the corrected blood stem cells could persist over the long term and produce the T cells that patients would need to lead healthy lives.
Ablation of CaMKIIδ oxidation by CRISPR-Cas9 base editing as a therapy for cardiac disease - ScienceCRISPR-Cas9 gene editing is emerging as a prospective therapy for genomic mutations. However, current editing approaches are directed primarily toward relatively small cohorts of patients wit
BigField GEG Tech's insight:
A novel CRISPR-Cas9 approach that targets a damaging signaling pathway in the heart confers protection against ischemia and reperfusion injury, according to a study in mice. The findings suggest that gene editing could offer a permanent, advanced strategy for treating heart disease and even serve as an intervention to repair heart damage immediately after a heart attack. CRISPR-Cas9 gene editing has shown promise as a therapeutic approach for the treatment of rare inherited diseases. Chronic overactivation of Ca2+/calmodulin-dependent protein kinase IIδ (CaMKIIδ) is known to cause several heart diseases in humans and mice, including lesions. The researchers found that using CRISPR-Cas9 adenine base editing to eliminate oxidative activation sites of the CaMKIIδ gene in cardiomyocytes protected them from IR injury in mouse models. In addition, the researchers found that injecting gene-editing reagents into mice shortly after IR injury allowed the animals to recover cardiac function after severe damage.
Bacterial abortive-infection systems limit the spread of foreign invaders by shutting down or killing infected cells before the invaders can replicate1,2. Several RNA-targeting CRISPR–Cas systems (that is, types III and VI) cause abortive-infection phenotypes by activating indiscriminate nucleases3–5. However, a CRISPR-mediated abortive mechanism that leverages indiscriminate DNase activity of an RNA-guided single-effector nuclease has yet to be observed. Here we report that RNA targeting by the type V single-effector nuclease Cas12a2 drives abortive infection through non-specific cleavage of double-stranded DNA (dsDNA). After recognizing an RNA target with an activating protospacer-flanking sequence, Cas12a2 efficiently degrades single-stranded RNA (ssRNA), single-stranded DNA (ssDNA) and dsDNA. Within cells, the activation of Cas12a2 induces an SOS DNA-damage response and impairs growth, preventing the dissemination of the invader. Finally, we harnessed the collateral activity of Cas12a2 for direct RNA detection, demonstrating that Cas12a2 can be repurposed as an RNA-guided RNA-targeting tool. These findings expand the known defensive abilities of CRISPR–Cas systems and create additional opportunities for CRISPR technologies. RNA targeting by the Sulfuricurvum type V single-effector nuclease SuCas12a2 drives abortive infection through non-specific cleavage of double-stranded DNA—after recognition of an RNA target through an activating protospacer-flanking sequence, SuCas12a2 efficiently degrades ssRNA, ssDNA and dsDNA.
BigField GEG Tech's insight:
Scientists at the Helmholtz Institute Würzburg in Germany, and Benson Hill, Inc. (Missouri) and Utah State University in the U.S., have found a nuclease, which they dubbed Cas12a2, that represents an entirely new type of CRISPR immune defense. Unlike any other previously known nuclease of the CRISPR-Cas immune system, the source of ‘gene scissors,’ Cas12a2 destroys DNA to shut down an infected cell. The findings could lead to new CRISPR technologies for molecular biology diagnostics, among other applications.
Researchers at VCU Massey Cancer Center have set their sights on a new therapeutic target for an aggressive form of breast cancer with limited treatment options.
BigField GEG Tech's insight:
Breast cancer is the second most common cancer in American women, and triple-negative breast cancer (TNBC) is a more aggressive and deadly form of the disease that accounts for 10-15% of all breast tumors. Using a comprehensive, state-of-the-art genomic screening method known as CRISPR/CAS9 screening, scientists were able to identify a specific enzyme called UBA1 that proved to be an ideal therapeutic target. Using a new UBA inhibitor drug called TAK-243, they blocked the cellular function of UBA1 and effectively killed cancer cells in patient-derived breast tumors in mice. Previous research has shown that UBA1 inhibitors can have a positive impact on hematological cancers such as acute myeloid leukemia and chronic myeloid leukemia. This study, recently published in PNAS Nexus, is the first to suggest that UBA1 inhibitors may be effective in TNBC. TAK-243 was recently tested in early phase trials, paving the way for potential testing in TNBC patients. The researchers also determined that the c-MYC gene can be harnessed to cooperate with TAK-243 to initiate a cellular stress response and improve the drug's ability to combat TNBC. This supports the idea that TAK-243 may be effective in TNBC with high c-MYC expression, where c-MYC may serve as a biomarker for drug response.
|






















In vivo screening of the CRISPR genome identifies the transcriptional modulator CITED2 as an essential factor in the progression of prostate cancer to bone metastases. The discovery not only improves understanding of the molecular basis of the disease, but also opens up new avenues for targeted therapies, potentially revolutionizing treatment paradigms for patients battling advanced prostate cancer. The study meticulously engineered non-metastatic human prostate cancer cell lines to activate or inhibit gene expression using CRISPRa or CRISPRi technology. Modified cancer cells were then implanted into the prostate of nude mice, and following tumor development and emergence of metastases, primary and metastatic tumors were harvested for analysis. In vivo CRISPR screening identified CITED2 as an important promoter of bone metastasis, standing out among various genes for its substantial impact. Subsequent functional validation experiments, including innovative organ-on-a-chip assays, reinforced CITED2's role in promoting bone invasion, highlighting its potential as a therapeutic target. The research also looked at CITED2-driven transcriptional profiles, revealing distinct patterns of primary and metastatic cancer, which could inform the development of precision medicine approaches.