The use of broad-spectrum antibiotics in the month leading up to chimeric antigen receptor T-cell therapy led to poorer outcomes and increased treatment-related toxicities, study results showed.Certain types of gut bacteria had an impact on treatment efficacy and related toxicities among patients who received CAR-T for non-Hodgkin lymphoma or acute lymphoblastic leukemia, researchers reported.
Get Started for FREE
Sign up with Facebook Sign up with X
I don't have a Facebook or a X account
 Your new post is loading... Your new post is loading...
 Your new post is loading... Your new post is loading...
Pierre-Luc Jellimann 's curator insight,
November 17, 2022 3:06 AM
CAR T cell immunotherapies are more effective as a treatment for patients with leukemia or B cell lymphomas because once they are re-injected into the patient, they migrate and lodge in the bone marrow and other organs that make up the lymphatic system. However, for solid tumours, such as breast cancer, the CAR T cells have difficulty migrating to the tumour because of the microenvironment that surrounds it. Recently, a study conducted by researchers at the UNC Lineberger Comprehensive Cancer Center, shows that adding a small molecule to the CAR T cell-based treatment could stimulate the Th17 and Tc17 cells of the immune system to effectively attack solid tumours. To stimulate the accumulation of these Th17 and Tc17 cells in the vicinity of solid tumours, the research team discovered that the stimulator of interferon agonist (STING) genes, cGAMP, activates the human STING and is known to stimulate the human immune system. The various experiments showed that mice injected with cGAMP showed increased proliferation of T cells and these cells migrated to the tumour site. The end result was a significant decrease in tumour growth and improved survival. |
|




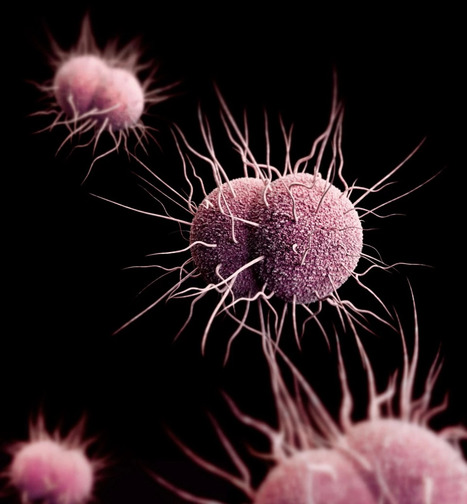








Researchers examined two cohorts of patients who received CD19-directed CAR-T cells for non-Hodgkin's lymphoma or B-cell acute lymphoblastic leukemia. The researchers used the first cohort to retrospectively examine the impact of prior antibiotic use on CAR-T clinical outcomes. The second cohort had prospective baseline fecal samples collected before CAR-T cell infusion for subsequent assessment of the fecal microbiome. The investigators determined that the use of certain antibiotics including piperacillin/tazobactam, meropenem, and imipenem/cilastatin, negatively affected OS (HR = 1.71; 95% CI, 1.12-2.59). The investigators also noted a significantly increased risk of immune effector cell-associated neurotoxicity syndrome among the entire cohort evaluated for pre-CAR-T antibiotic use (P = 0.023). Stool samples from the prospective cohort demonstrated an altered fecal microbiome including lower alpha diversity, increased frequency of bacterial dominance, and altered bacterial composition compared with healthy controls. The results of this study suggest that the composition of the gut microbiome affects CAR-T outcomes, but the investigators cautioned that further prospective studies in larger patient populations are needed to confirm the associations.