Mayo Clinic scientists have developed an immunotherapy strategy that potentially lays the groundwork for treating a spectrum of autoimmune diseases.
Research and publish the best content.
Get Started for FREE
Sign up with Facebook Sign up with X
I don't have a Facebook or a X account
Already have an account: Login
 Your new post is loading... Your new post is loading...
 Your new post is loading... Your new post is loading...
Pierre-Luc Jellimann 's curator insight,
November 4, 2022 6:58 PM
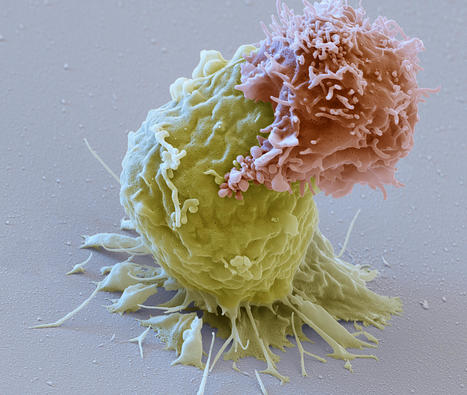
Mass General investigators have created a new method that could make immune therapy more effective again brain tumors and expand its use against other types of solid tumors. Their study is published in the journal Nature Biotechnology. |
Pierre-Luc Jellimann 's curator insight,
October 26, 2022 9:01 AM
Découverte d'un vaccin thérapeutique utilisant les cellules cancéreuses (dénaturées) du patient afin d'entrainer le SI à reconnaitre et à éradiquer les cellules cancéreuses + mise en place d'une mémoire immunitaire sur plusieurs mois. Effet concluant chez des souris ayant un mélanome.
|







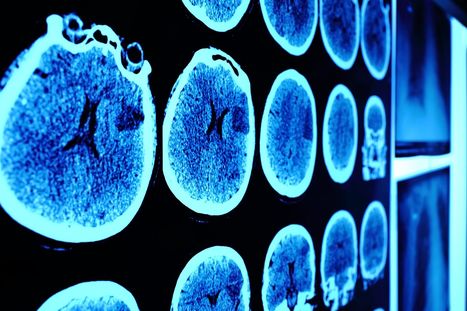











Graft-versus-host disease occurs when a donor's cells attack the recipient's tissues, usually following a bone marrow or stem cell transplant. In a recent study, a new technique involving the combination of Chimeric Antigen Receptors (CARs) with Mesenchymal Stromal Cells (MSCs), resulting in modified stem cells known as CAR-MSCs, was used to specifically target a protein linked to graft-versus-host disease, but also to inflammatory bowel diseases such as ulcerative colitis and Crohn's disease. In mouse models, when stimulated by the specific protein for which they were designed, CAR-MSCs showed an enhanced ability to reach the inflamed area, better control inflammation and improve outcome and survival. This was mediated by a change in the genetic signature of CAR-MSCs, the proteins they released and receptor expression. These preliminary results pave the way for future applications of this technology, paving the way for improving the versatility of the therapy to treat various diseases across the autoimmune spectrum.